Best disease, also known as vitelliform macular dystrophy, is an autosomal dominant hereditary disorder caused by mutations in the BEST1 (VMD2) gene. It often affects both eyes simultaneously or sequentially and is most commonly observed in children and adolescents, with an equal incidence in males and females. Visual acuity in the early stages is typically normal or mildly reduced, though severe cases may result in vision limited to counting fingers. Visual acuity between the two eyes is often asymmetric.
Clinical Features
The disease is classified into four stages based on its progression:
Pre-Vitelliform Stage
Fundus examination appears normal, or there may be small yellowish dots at the center of the fovea resembling a honeycomb pattern. Visual acuity remains unaffected.
Vitelliform Stage
This stage typically occurs between the ages of 3 and 15. Visual acuity is often normal. The macula develops a distinct lesion resembling an egg yolk or orange, with a well-defined circular or near-circular shape, measuring about 0.5–3 disc diameters (DD) in size. The lesion is mildly elevated, with its center resembling the intact yolk of a fried egg, surrounded by a darker rim. Retinal vessels are visible traversing the lesion.
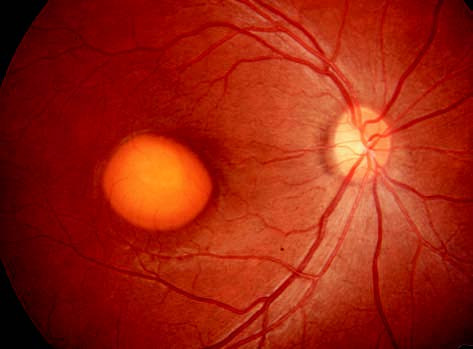
Figure 1 Fundus photograph of the right eye with Best disease.
The macula shows a near-circular, well-defined lesion resembling an egg yolk, measuring approximately 2 disc diameters in size. The lesion is slightly elevated, has a dark rim, and retinal vessels are seen traversing over it.
Vitelliruptive Stage
Visual acuity decreases significantly. Fundus examination reveals fragmented vitelliform material, producing an appearance similar to a broken egg yolk or scrambled eggs, with an irregular shape. In some cases, the vitelliform material dehydrates, condenses, and settles downward due to gravity, resulting in a fluid-filled upper layer with a fluid level visible. A minority of patients may develop choroidal neovascularization (CNV), leading to severe vision impairment.
Atrophic Stage
In the late stages, retinal and choroidal atrophy occurs, accompanied by pigmentary loss or pigmentation. Permanent visual damage is common at this stage, often associated with an absolute central scotoma.
Diagnosis
Fundus Fluorescein Angiography (FFA)
In the intact vitelliform stage, the lesion typically shows persistent hypofluorescence (fluorescence masking). During the vitelliruptive stage, a mixed pattern of transmission fluorescence and fluorescence masking is observed. In the atrophic stage, background fluorescence is diminished, and large choroidal vessels become visible. Fluorescein leakage may occur in cases with neovascularization.
Electrophysiology Testing
Electroretinography (ERG) is normal, but electro-oculography (EOG) is characteristically abnormal, showing a significantly reduced light-peak-to-dark-trough ratio (Arden ratio), usually below 1.5. This finding is critical for diagnosis and differentiation from other conditions.
Fundus Autofluorescence (FAF)
Typical cases reveal strong autofluorescence at the lesion site.
Treatment
No definitive treatment is currently available. Management focuses on addressing potential complications such as CNV when they arise. Gene therapy is under investigation.