Stargardt disease is the most common form of juvenile macular dystrophy. It is typically caused by mutations in the ABCA4 gene and follows an autosomal recessive inheritance pattern, with no gender or racial predisposition. The disease usually manifests between the ages of 6 and 20. The most common symptoms include progressive, bilateral, symmetrical vision loss, which may be accompanied by photophobia, color vision abnormalities, central scotomas, and impaired dark adaptation. The characteristic fundus appearance features an oval-shaped atrophic lesion centered on the macula with scattered yellow flecks (round or pisciform) in the surrounding retina. If the flecks are widespread without macular involvement, the condition is referred to as fundus flavimaculatus. These two presentations may represent different manifestations of the same disease.
Clinical Features
Symmetry
The disease affects both eyes symmetrically, with best-corrected visual acuity typically ranging between 0.1 and 0.25.
Fundus Findings
Early in the disease, the fundus may appear entirely normal. Over time, the foveal reflex disappears, and a horizontally oval-shaped atrophic region measuring approximately 2 × 1.5 disc diameters (DD) develops symmetrically in the macular region. This area may exhibit a metallic, foil-like sheen in some cases, with scattered yellow flecks surrounding the atrophy. In advanced stages, the macula appears to have a bronze-like sheen, with atrophy resembling a map-like pattern, and pigment clumps may be present. Large and medium-sized choroidal vessels as well as white sclera become exposed beneath the areas of atrophy.
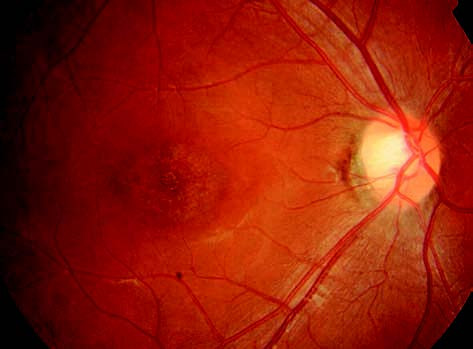
Figure 1 Fundus photograph of the right eye with Stargardt disease.
The macular region displays a horizontally oval-shaped area of atrophy with the absence of the central foveal reflex.
Diagnosis
Fundus Fluorescein Angiography (FFA)
Early cases display punctate hyperfluorescence within the central macula, distributed in an oval-shaped pattern. Some cases exhibit the "choroidal silence sign," indicating compromised choroidal fluorescence. As the disease progresses, the number of yellow flecks increases in the posterior pole. Most flecks show hyperfluorescence caused by window defects (transmission fluorescence), with a few showing blocked fluorescence. In advanced stages, large choroidal vessels become visible against a hypofluorescent background in atrophic regions.
Optical Coherence Tomography (OCT)
Examination reveals photoreceptor loss and outer retinal atrophy in the macular region. In advanced cases, the foveal neurosensory epithelium significantly thins or disappears entirely, with accompanying thinning of both the retina and choroid.
Fundus Autofluorescence (FAF)
This method offers characteristic findings, including a hyperautofluorescent background. The atrophic area in the central macula appears hypoautofluorescent, while surrounding flecks show scattered hyperautofluorescence.
Differential diagnosis is important in early cases, as Stargardt disease may be misdiagnosed as amblyopia. Other conditions to consider include cone-rod dystrophy, vitelliform macular dystrophy, and other forms of macular dystrophy.
Treatment
No effective treatment currently exists. Patients with severe vision loss may benefit from assistive devices or low vision rehabilitation. Gene therapy and stem cell therapy are being actively investigated in clinical trials.