Rhegmatogenous retinal detachment occurs when liquefied vitreous passes through a retinal tear and accumulates beneath the retinal neurosensory layer, causing separation between the neurosensory retina and the retinal pigment epithelium (RPE).
Etiology and Pathogenesis
The two key factors contributing to rhegmatogenous retinal detachment are:
- Formation of retinal tears.
- Vitreous traction and liquefaction.
Retinal tears are associated with factors such as retinal degeneration, posterior vitreous detachment (PVD), and vitreoretinal traction. Retinal degeneration, commonly located in the peripheral retina, includes lattice degeneration, snail track degeneration, cystic degeneration, and retinoschisis. Degenerated retinal tissue may result in small atrophic round holes, which do not cause retinal detachment unless accompanied by vitreous traction. Vitreous liquefaction and PVD can cause repetitive traction at sites of vitreous attachment to the retina, leading to horseshoe-shaped tears, often accompanied by a flap of elevated retina adherent to the vitreous. Following blunt ocular trauma, vitreoretinal traction may result in retinal breaks at the ora serrata. Once a tear forms with vitreoretinal traction, liquefied vitreous can enter beneath the neurosensory retina, inducing retinal detachment.
Rhegmatogenous retinal detachment tends to occur more frequently in older individuals, patients with high myopia, aphakic or pseudophakic eyes, and those with a history of ocular trauma.
Clinical Presentation
During the early stages, symptoms may include floaters, photopsia (flashing lights), and curtain-like visual field defects corresponding to the area of retinal detachment. These symptoms may gradually worsen. In cases where detachment involves the macula, a marked decline in visual acuity occurs.
Fundus examination reveals elevated grayish-white detached retina. The extent of detachment may range from localized areas to total retinal detachment. In extensive detachment, the retina appears uneven and undulates like waves. Severe cases may exhibit retinal surface proliferation with fixed retinal folds.
Diagnosis
Ultra-Widefield Fundus Photography
This method provides an overview of the extent of retinal detachment and can assist in identifying obvious retinal tears or regions with suspected retinal degeneration. It is a rapid, non-contact, and non-invasive diagnostic tool.
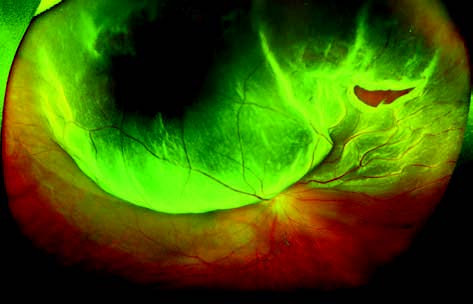
Figure 1 Ultra-widefield fundus photograph of rhegmatogenous retinal detachment in the right eye
The detached retina appears as an elevated bluish-gray region, involving the central macula. A "horseshoe-shaped" tear is visible in the superior-nasal retina.
Ocular Ultrasonography
In cases where optical clarity is poor, ultrasound can provide an approximate assessment of retinal detachment. The addition of Doppler signals enhances diagnostic accuracy for retinal detachment.
Post-Dilation Fundus Examinations
Techniques such as fundus contact lens examination, indirect ophthalmoscopy, or three-mirror lens examination are essential for delineating the extent of detachment and accurately locating retinal tears. In necessary cases, a scleral depression examination can facilitate the identification of peripheral retinal tears anterior to the equator. Tears are most commonly found in the superior temporal quadrant, followed by the inferior temporal, and nasal regions. On a background of grayish detached retina, retinal tears appear red. Retinal tears in aphakic or pseudophakic eyes, as well as in cases of chronic inferior retinal detachment, may be less conspicuous.
Treatment Principles
The goals of treatment are to seal retinal tears and to reattach the retina. Preoperative and intraoperative identification and accurate localization of all tears are crucial. Surgical options include scleral buckling, explant-based procedures, or vitreoretinal surgery for more complex cases. Retinal tears can be sealed using laser photocoagulation or cryotherapy around the tear. The inflammatory response induced by these treatments promotes adhesion between the neurosensory retina and RPE, effectively sealing the tear. Visual prognosis depends on whether the macula is involved and the duration of detachment. Cases without macular detachment or with a short duration of detachment (<1 week) tend to have better visual outcomes.