An epiretinal membrane refers to a thin, fibrous cell membrane formed on the vitreoretinal interface, primarily due to the migration and proliferation of retinal glial cells and retinal pigment epithelial (RPE) cells. While epiretinal membranes can form on any part of the retina, those occurring in or near the macula are known as macular epiretinal membranes (ERM), or simply macular membranes. The development of macular ERM has been associated with several factors, including:
- Postoperative changes, such as those occurring after retinal detachment surgery, vitreoretinal surgery, or retinal photocoagulation or cryotherapy.
- Certain inflammatory ocular conditions, including endophthalmitis and retinal vasculitis.
- Hemorrhagic retinal vascular diseases.
- Ocular trauma.
Idiopathic macular membranes are commonly observed in older individuals without other signs of eye disease and are often associated with posterior vitreous detachment.
Macular membranes can be divided into two categories based on their progression and clinical presentation:
- Cellophane maculopathy: This form is more common and typically idiopathic, involving a thin, transparent membrane on the surface of the macular retina. Visual acuity in the affected eye is normal or only slightly reduced, with minor visual distortion. On fundus examination, the macular area appears with irregular or shiny reflexes, resembling a layer of cellophane. As the membrane thickens and contracts, retinal surface striae and distortion of small blood vessels may develop.
- Macular pucker: This form results from further thickening and contraction of the membrane and can be either idiopathic or secondary. Significant reduction in vision (≤0.5 in decimal Snellen acuity) and noticeable visual distortion may occur. Fundus examination usually reveals a grayish-white fibrous membrane with unclear boundaries in the posterior pole, retinal wrinkling, and severe distortion of macular retinal vessels, sometimes displaced centrally. Macular edema or shallow detachment may be present, along with ectopia.
OCT imaging demonstrates a linear high-reflective signal from the macular membrane, with distortion and elevation of the central fovea. Splitting of the retinal layers or even macular hole formation may also be observed in some cases. FFA imaging reveals features such as pronounced vascular distortion and leakage.
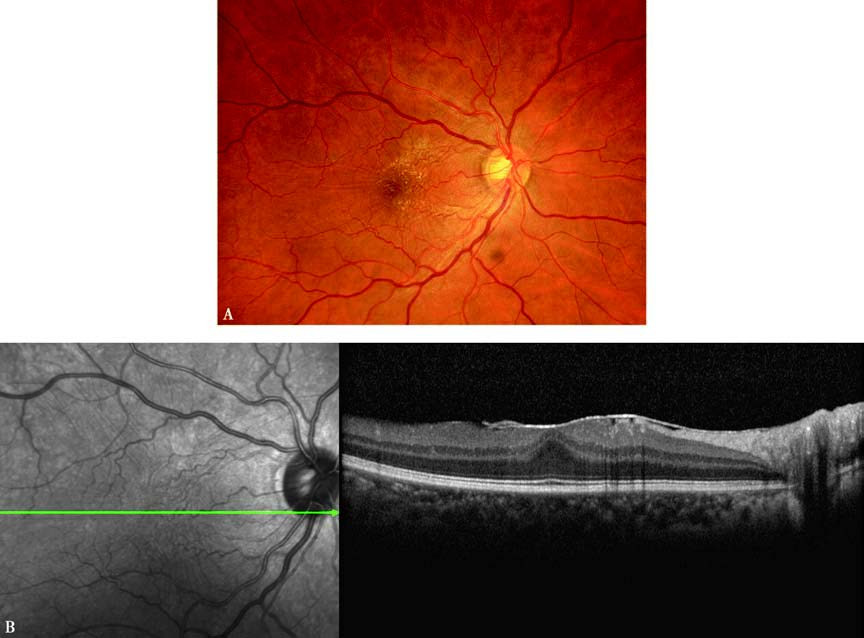
Figure 1 Appearance of macular ERM in the right eye
A. Fundus photography shows irregular yellowish-white reflexes in the macular region, with surface striae and vascular distortion.
B. OCT horizontal scan (aligned with the green line) reveals a linear high-reflective signal on the macula and elevation of the central fovea.
Currently, no effective pharmacological treatments are available for macular epiretinal membranes. In cases where mild visual acuity decline occurs, treatment may not be required. For those with progressive vision loss or significant visual distortion, vitrectomy combined with membrane peeling may be performed. This procedure often alleviates the distortion and improves visual acuity in approximately 50% of cases.