Choroidal neovascularization (CNV) is a common pathological feature shared by numerous diseases. Its underlying mechanism remains unclear, though it is generally believed to be associated with the disruption of the integrity of the RPE-Bruch's membrane-choriocapillaris complex. The causes include degenerative changes, inflammation, trauma, and idiopathic factors. Additionally, CNV may be secondary to hereditary retinal diseases, tumors, chronic central serous chorioretinopathy (CSC), and other conditions. CNV typically occurs in the macular region, leading to a series of pathological changes such as hemorrhage, exudation, and scar formation, which compromise the structure and function of the eye and severely impair visual function. More than 40 diseases are associated with CNV, which represents a significant cause of vision loss. The most common CNV-related conditions in clinical practice include wet age-related macular degeneration (AMD) and pathological myopic maculopathy.
Clinical Manifestations
CNV can occur in individuals across all age groups and may involve one or both eyes. Patients often seek medical attention due to symptoms such as decreased vision, visual distortion, and central scotomas. Fundus examination reveals a grayish-white lesion in the macular region, often surrounded by associated findings such as hemorrhage, edema, and exudation. The size of the CNV lesion varies according to the underlying cause, and accompanying manifestations of the primary disease can also be observed in the fundus. Fluorescein fundus angiography (FFA) typically shows intense fluorescence due to leakage from the neovascular structures, while indocyanine green angiography (ICGA) provides detailed visualization of CNV morphology. Optical coherence tomography (OCT) reveals irregular, clumped, hyperreflective signals located under the RPE layer or penetrating through the RPE into the subretinal space, often accompanied by neurosensory retinal detachment in the surrounding area. OCT angiography (OCTA) detects a dense vascular network with high blood flow signals in the macular region indicative of CNV.
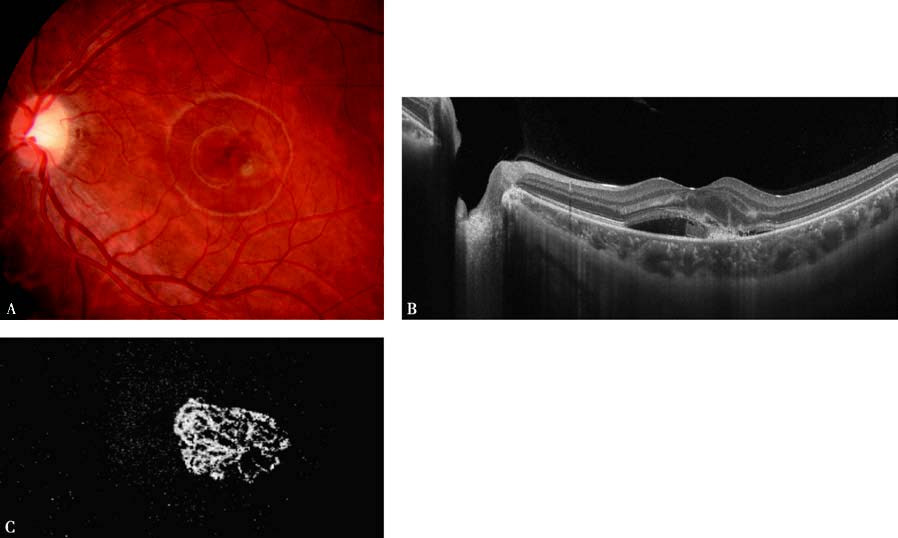
Figure 1 Features of idiopathic choroidal neovascularization in the left eye
A. Fundus photograph shows a grayish-white lesion in the subfoveal region, inferior temporal to the macula, with surrounding hemorrhage and edema.
B. OCT reveals irregular, clumped, hyperreflective signals above the RPE layer, accompanied by neurosensory detachment in the surrounding area.
C. OCTA shows the neovascularization exhibiting a "tangled ball" appearance.
Treatment
Treatment should begin with addressing the underlying cause. Significant progress has been made in the treatment of CNV in recent years. Intravitreal injections of anti-VEGF agents have become the first-line therapeutic strategy. Approved anti-VEGF drugs for CNV treatment include ranibizumab and conbercept. For patients with associated inflammatory changes, corticosteroids may be administered topically or systemically. Photodynamic therapy (PDT) and laser photocoagulation may be appropriate for certain CNV-related diseases. Research into gene therapy is ongoing.