Diabetic retinopathy (DR) is the most common retinal vascular disease encountered in clinical practice and is one of the leading causes of blindness among working-age populations. In its early stages, DR is asymptomatic, but as the disease progresses, varying degrees of vision loss gradually develop. Traditionally, DR has been considered primarily a microvascular disease. However, recent studies suggest that it also involves neurodegenerative processes. Structural disruption and functional impairment of the neurovascular unit (NVU)—comprising the functional coupling of retinal vascular endothelial cells, neurons, and glial cells—play a crucial role in the onset and progression of DR.
Clinical Stages or Classifications
Diabetic retinopathy is classified into two types according to the stage of disease development and severity: nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR). Both types can involve diabetic macular edema (DME).
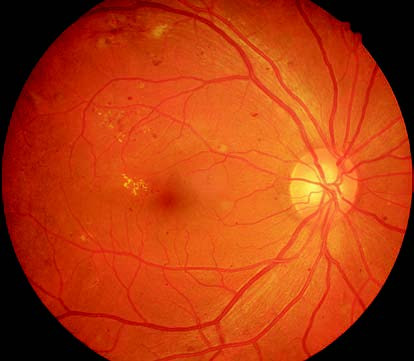
Figure 1 Color fundus photograph of the right eye with nonproliferative diabetic retinopathy
The posterior pole of the retina displays scattered microaneurysms, hemorrhages, and yellow-white hard exudates.

Figure 2 Color fundus photograph of the left eye with proliferative diabetic retinopathy
Retinal neovascularization and fibrous proliferation are visible, accompanied by tractional retinal detachment.
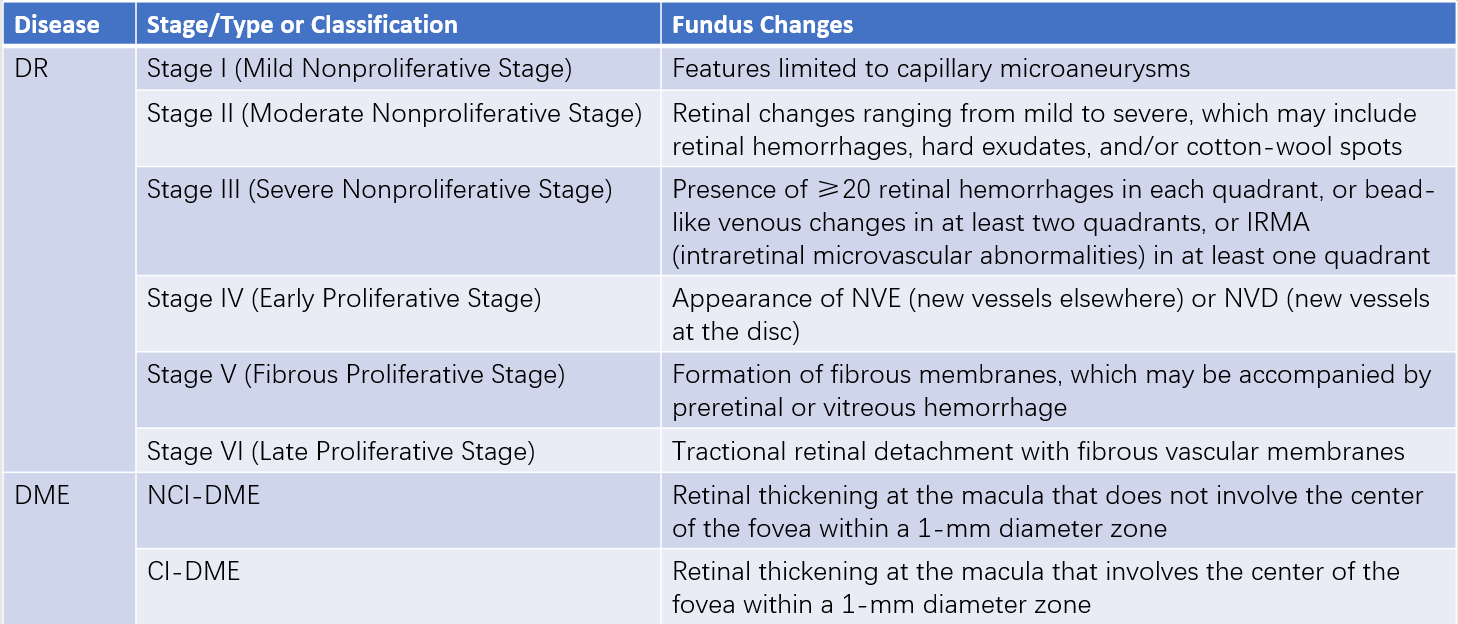
Table 1 Classification and staging of diabetic retinopathy and diabetic macular edema
Notes:
DR: Diabetic Retinopathy
DME: Diabetic Macular Edema
IRMA: Intraretinal Microvascular Abnormalities
NVE: New Vessels Elsewhere
NVD: New Vessels at the Disc
NCI-DME: Non-Center-Involving Diabetic Macular Edema
CI-DME: Center-Involving Diabetic Macular Edema
DME refers to retinal thickening at the macular center due to capillary leakage resulting from disruption of the blood-retinal barrier. It primarily affects central vision. Based on the latest international classification (2017), DME is divided into two subtypes depending on whether the foveal center is involved: non-center-involving DME (NCI-DME) and center-involving DME (CI-DME).
Treatment
Management includes systemic disease control and local ocular treatment. It is essential to control blood glucose, blood pressure, and blood lipids in an evidence-based manner. Local ocular treatments include retinal laser photocoagulation, anti-vascular endothelial growth factor (anti-VEGF) therapy, corticosteroid injections, and surgical interventions.
For mild to moderate NPDR, observation is typically the primary approach. In cases of severe NPDR and PDR, panretinal photocoagulation (PRP) or PRP combined with intravitreal anti-VEGF therapy is administered to inhibit the formation of neovascularization, promote the regression of existing neovascular vessels, and prevent further disease progression. For cases of long-standing non-resorbing vitreous hemorrhage, tractional retinal detachment, or when the macula is involved, vitrectomy, possibly in combination with PRP and anti-VEGF therapy, is performed.
For DME, anti-VEGF agents have become the first-line treatment for CI-DME. For NCI-DME, focal or grid laser treatment may be considered, either alone or in combination with anti-VEGF therapy. When there is a poor or non-existent response to anti-VEGF agents, switching to intravitreal corticosteroid therapy may be considered. Intravitreal injections of anti-VEGF agents and/or sustained-release corticosteroids effectively reduce retinal vascular leakage, resolve macular edema, and improve visual acuity. Micropulse laser treatment is also effective for DME with a central retinal thickness (CRT) of less than 400 μm in the macular region.