Retinal periphlebitis, also known as Eales disease, is a significant retinal vascular disorder that causes vision loss in young adults.
Etiology
The etiology of this condition remains unknown. It is rare in Western countries but relatively common in China, India, and some parts of the Middle East. Due to its regional distribution, it has been previously associated with tuberculosis infection, as some patients test positive in the tuberculin skin test.
Clinical Manifestations
The condition primarily affects young males and typically involves both eyes sequentially. Early symptoms include blurred vision and the sensation of floaters in the visual field. As an idiopathic occlusive vascular disease of the peripheral retina, it affects both small arteries and veins, leading to areas of non-perfusion and/or neovascularization. Vitreous hemorrhage can occur suddenly, causing a painless and abrupt loss of vision in the affected eye, which may be reduced to light perception or finger counting. Hemorrhages tend to resolve relatively quickly, with partial recovery of vision, but recurrent vitreous hemorrhages are common. These recurrent episodes can ultimately result in tractional retinal detachment and blindness.
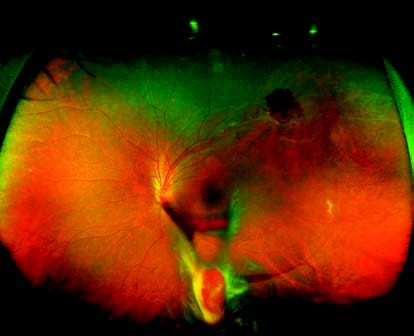
Figure 1 Ultra-widefield fundus photograph of Eales disease in the left eye
The peripheral retina in the superotemporal region of the left eye shows tortuous and dilated venules with perivascular sheathing, accompanied by superficial retinal hemorrhages. The inferior vitreous cavity contains hemorrhagic opacities, with evidence of partial blood organization.
Fundus examination reveals lesions predominantly located in the peripheral retina. Affected retinal venules are dilated and tortuous, surrounded by perivascular sheathing, and accompanied by superficial retinal hemorrhages. Hemorrhages may enter the vitreous cavity, causing varying degrees of vitreous opacity. Recurrent hemorrhages may lead to fibrovascular proliferation or tractional bands, and severe cases may progress to tractional retinal detachment. On fluorescein fundus angiography (FFA), findings include staining of the walls of affected venules, capillary dilation, fluorescein leakage, extensive areas of peripheral capillary non-perfusion, and the formation of neovascular membranes.
Treatment
The underlying cause should be investigated, and any associated inflammatory conditions should be treated. Corticosteroids can be administered orally or via peribulbar injection. Symptomatic treatment is recommended for fresh hemorrhages. Once vitreous hemorrhages have largely resolved, laser photocoagulation of the peripheral retinal lesions can be performed under the guidance of FFA. This treatment aims to eliminate non-perfusion areas, promote the regression of neovascularization, and reduce the risk of further hemorrhage. For severe vitreous hemorrhages that show no improvement after 4 to 6 weeks or in cases of tractional retinal detachment, vitrectomy is indicated.