The most common parasitic infection of the vitreous is Cysticercosis cellulosae. Eggs and scolex segments of tapeworms penetrate the intestinal mucosa and reach the eye through the bloodstream. The cysticercus initially lodges in the choroid, then moves into the subretinal space, and eventually penetrates the retina to enter the vitreous cavity.
Clinical Manifestations
Symptoms
When the parasite is alive, the inflammatory response tends to be mild, and patients may occasionally perceive shadows of its deforming, writhing movements. After the parasite dies, toxic endophthalmitis often develops, leading to significant vision loss.
Fundus Examination
Yellowish-white, semi-translucent, circular cysticerci may appear in the subretinal space or vitreous cavity. The size of the cysticerci typically ranges from 1.5 to 6 disc diameters (DD). Strong illumination may stimulate the head of the cysticercus to exhibit retractile movements, and a dense yellowish-white dot can often be observed when the scolex withdraws into the cystic body. The parasite can induce inflammation in surrounding tissues, potentially causing retinal detachment when located in the subretinal space or vitreous opacities after entering the vitreous cavity.
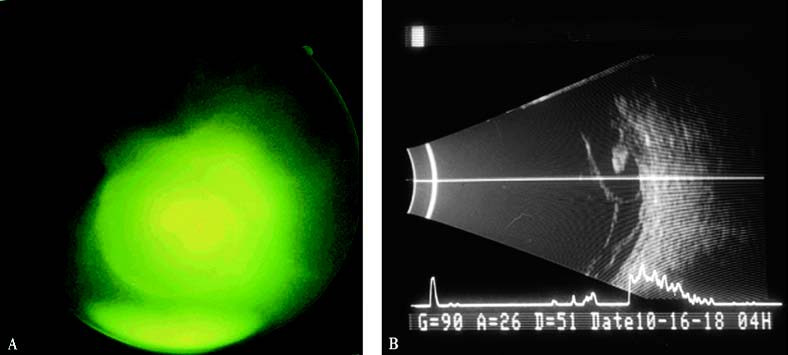
Figure 1 Vitreal Cysticercosis
A. Yellowish-white, semi-translucent, circular cysticercus in the vitreous cavity.
B. B-scan ultrasound image of the same patient.
Diagnosis
The diagnosis is made based on the characteristic appearance of the intraocular parasite. In uncertain cases, an ELISA test for tapeworm antibodies may be performed.
Treatment
Cysticerci located in the peripheral subretinal space may be removed through a scleral approach, while those in the vitreous cavity may be extracted via vitrectomy.