Congenital cataracts refer to cataracts that are present at or shortly after birth, or those that gradually develop within the first year of life due to congenital genetic or developmental disorders. Congenital cataracts are a common childhood eye disease and a significant cause of childhood blindness and amblyopia. The prevalence of congenital cataracts in newborns is approximately 0.5%. These cataracts may be familial or sporadic, unilateral or bilateral, and are sometimes accompanied by other congenital abnormalities affecting the eyes or the entire body.
Etiology
The causes of congenital cataracts can be classified into three main categories: genetic factors, environmental factors, and unknown factors.
Genetic Factors
Approximately half of congenital cataract cases are associated with genetic causes. There are four modes of inheritance for hereditary congenital cataracts: autosomal dominant (AD), autosomal recessive (AR), X-linked recessive (XR), and mitochondrial DNA inheritance, with the AD type being the most common. Most hereditary cataracts are caused by gene mutations, with fewer cases resulting from chromosomal abnormalities or mitochondrial disorders. Hereditary congenital cataracts exhibit significant genetic heterogeneity, meaning the same gene mutation may result in varied clinical presentations, while identical clinical manifestations may arise from mutations in different pathogenic genes.
Environmental Factors
Environmental factors represent another major cause of congenital cataracts. During the first trimester of pregnancy, when the fetal lens capsule has not fully developed and cannot resist viral infections, lens protein synthesis is highly active. Viral infections during this period can severely impair the growth and development of fetal lens epithelial cells and disrupt lens metabolism, leading to abnormal protein synthesis and lens opacities. Among the various causative viruses, rubella virus is the most common cause of congenital cataracts in fetuses, followed by infections such as varicella, herpes simplex, measles, herpes zoster, and influenza.
Other contributing factors include maternal malnutrition during pregnancy, pelvic radiation exposure, use of certain medications (e.g., high-dose tetracyclines, hormones, salicylates, anticoagulants), systemic diseases (e.g., heart disease, nephritis, diabetes, anemia, hyperthyroidism, tetany), or vitamin D deficiency. Congenital cataracts can also occur in preterm infants or as a result of intrauterine hypoxia.
Unknown Causes
Many sporadic cases lack a definitive identification of genetic or environmental factors. Some cases may be genetic in origin but remain undiagnosed due to the absence of a family history, potentially caused by a first-generation de novo dominant gene mutation. Similarly, some autosomal recessive cases may develop without a clear determination of genetic inheritance.
Clinical Manifestations
Congenital cataracts may affect one or both eyes. Most cases are static, while a few progress after birth. Classification often depends on the location, morphology, and extent of lens opacities. Congenital cataracts exhibit diverse clinical manifestations based on these characteristics, including but not limited to membranous, nuclear, perinuclear, anterior polar, posterior polar, dust-like, punctate, disciform (Coppock cataracts), sutural, coral-like, corona-like, liquified hard nucleus, and total cataracts.

Figure 1 Congenital cataract (blue clustered opacity)
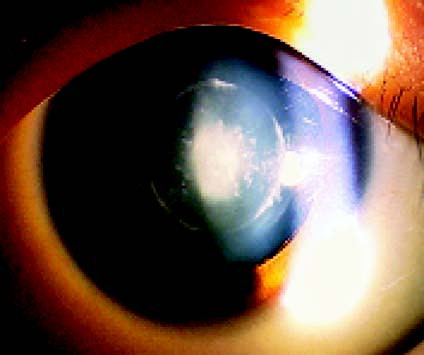
Figure 2 Congenital cataract (nuclear dust-like opacity)
Diagnosis
The diagnosis is generally based on the medical history and the morphological features of lens opacities. For congenital cataracts accompanied by other systemic anomalies, appropriate laboratory tests should be performed depending on individual circumstances. Blood glucose, urine glucose, and ketones should be examined in cases of diabetes or neonatal hypoglycemia. Patients with concomitant renal disease should undergo urinalysis and tests for urine amino acids. If metabolic diseases are suspected, blood amino acid levels should be measured. Additional diagnostic options include testing for urinary phenylpyruvate, screening for homocystinuria, and screening for galactosuria.
Treatment
The primary goal of treating congenital cataracts is to restore vision and reduce the incidence of amblyopia and blindness.
For cases that minimally impact vision, such as anterior polar cataracts, corona-like cataracts, and punctate cataracts, treatment is generally not required, with regular follow-up and observation being sufficient.
For cases that significantly impair vision, such as total cataracts or perinuclear cataracts, surgical intervention may be necessary. Procedures such as membranectomy can be used for membranous cataracts. Earlier surgery increases the likelihood of achieving good visual outcomes for the child. In cases of unilateral cataracts that severely affect vision, cataract removal surgery is typically performed 4–6 weeks after birth, depending on the infant's overall health and ability to undergo anesthesia. For bilateral total cataracts or cataracts with central visual axis opacities, surgery within the first 10 weeks of life has a better visual prognosis. For bilateral cases, surgery on the second eye is usually performed 2–4 weeks after the first surgery.
Aphakic eyes require refractive correction and visual training to prevent amblyopia and enhance fusion function development. Common correction methods include:
- Eyeglasses: Simple, easy to replace or adjust.
- Contact Lenses: Suitable for most cases of unilateral aphakic eyes, though frequent handling increases the risk of corneal epithelial damage and infection.
- Intraocular Lens (IOL) Implantation: Advances in microsurgical techniques and improvements in IOL quality have reduced the risk of serious postoperative complications. Considering the development of the infant's eye, IOL implantation is generally recommended around the age of 2 years.