Dry eye is the most common ocular disease after refractive errors. In recent years, the incidence of dry eye has increased globally. This rise can be attributed to widespread use of video display terminals, such as smartphones and computers, the development of unhealthy lifestyle habits such as staying up late, the acceleration of population aging, and the increasing prevalence of chronic systemic conditions such as diabetes, hyperlipidemia, and depression or anxiety. These factors have led to a year-on-year increase in the number of individuals affected by dry eye. Additionally, with the growing use of video display terminals among younger populations, the condition is trending toward a younger demographic.
Dry eye, also known as keratoconjunctivitis sicca, is a chronic ocular surface disease caused by multiple factors. It results from abnormalities in the quality, quantity, or dynamics of tears that lead to tear film instability or an imbalance in the ocular surface microenvironment. It may be accompanied by ocular surface inflammation, tissue damage, and neural dysfunction, causing a range of ocular discomfort symptoms and/or visual impairment.
Causes and Classification
Dry eye has a wide variety of causes. The lacrimal glands, ocular surface (including the cornea, conjunctiva, and meibomian glands), eyelids, and the sensory and motor nerves that connect these structures together form a functional unit. Any disruption to this unit may contribute to the development of dry eye. The main contributing factors include:
- Environmental Factors: Dry environments, air conditioning or heating, high altitudes, windy or dusty conditions, and air pollution (e.g., smog).
- Lifestyle Factors: Prolonged viewing of video display terminals, contact lens use, eye makeup, and sleep disorders.
- Systemic and Local Diseases: Local ocular conditions such as blepharitis, meibomian gland dysfunction (MGD), allergic conjunctivitis, and incomplete eyelid closure, as well as systemic diseases like autoimmune disorders, diabetes, decreased levels of sex hormones, and long-term use of medications such as anti-anxiety drugs.
The pathological processes of dry eye are complex, which is one of the key reasons why its classification remains incomplete. In 2017, the International Tear Film and Ocular Surface Society (TFOS) divided dry eye into three types: aqueous tear deficiency (ATD), evaporative, and mixed types.
- Aqueous Tear Deficiency (ATD): This type results from lacrimal gland diseases or dysfunction, which lead to insufficient tear production. It is further categorized into Sjögren syndrome-associated aqueous tear deficiency (SS-ATD) and non-Sjögren syndrome aqueous tear deficiency (non-SS-ATD) based on the underlying cause.
- Evaporative Type: This is primarily associated with meibomian gland dysfunction (MGD), which affects the lipid layer of the tear film, leading to excessive tear film evaporation.
Clinical Manifestations and Examinations
Symptoms and Questionnaire Surveys
The symptoms of dry eye lack specificity. Common symptoms include dryness, foreign body sensation, burning, itching, pain, redness, visual fatigue, blurred vision, and visual fluctuations. Some patients may find it difficult to describe their discomfort precisely, only referring to it as “ocular discomfort.” When dry eye is associated with systemic diseases, symptoms such as dry mouth, joint pain, or skin lesions may also be present. Based on the common symptoms of dry eye and its related disease history, questionnaires have been designed to quantify responses for determining the presence of dry eye. Commonly used questionnaires include the Ocular Surface Disease Index (OSDI) and the Standard Patient Evaluation of Eye Dryness (SPEED), which provide a simple and practical primary assessment for dry eye.
Examination of Tear Secretion
Schirmer Test
This involves using Schirmer test strips (5 mm × 35 mm) with one end folded 5 mm and placed into the conjunctival sac at the junction of the lateral and middle thirds of the lower eyelid. The length of the strip moistened by tears is measured after 5 minutes. The recommended diagnostic cutoff value is Schirmer I test ≤10 mm/5 min (without anesthesia).
Tear Meniscus Height Assessment
Using a slit lamp microscope, the concave arc of tear fluid at the junction of the eyelid margin is observed, and the height of tear retention is measured indirectly to evaluate tear secretion. A height of ≤0.35 mm is indicative of reduced tear secretion.
Phenol Red Thread (PRT) Test
A phenol red-impregnated cotton thread is placed in the temporal conjunctival sac for 15 seconds, and the length of the thread that changes color due to tear wetting is measured. A length of ≤20 mm indicates reduced tear secretion.
Examination of Tear Film Stability
Tear film breakup time (BUT) is currently the most commonly used method. It is conducted in an environment with appropriate temperature, humidity, and minimal light interference. The standard procedure involves instilling a small amount (less than 2 μL) of a 1% fluorescein sodium solution into the conjunctival sac or applying fluorescein-impregnated paper moistened with saline to the inferior conjunctiva. The patient is asked to blink several times to ensure an even distribution of the dye on the ocular surface. The time from the last complete blink to the appearance of the first dark spot on the cornea is recorded as the tear film breakup time, with the test conducted three times to calculate an average value. The recommended diagnostic cutoff value is ≤5 seconds.
Ocular Surface Epithelial Staining
Fluorescein Staining
A small amount of fluorescein sodium solution or a moistened fluorescein strip is applied to the inferior conjunctiva. Under cobalt blue light from a slit lamp microscope, fluorescein staining is observed. Healthy corneal epithelium does not stain, while damaged epithelium stains green. Staining may appear as punctate or diffuse areas under cobalt blue light, with the staining extent correlating with the severity of ocular surface damage. This staining method is used as an index to evaluate epithelial barrier function and integrity, as well as dry eye severity.
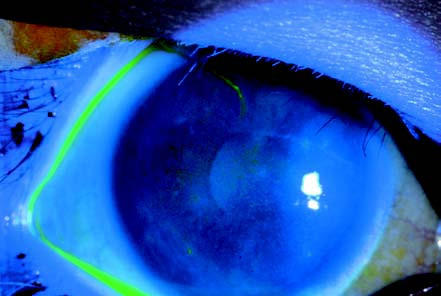
Figure 1 Corneal fluorescein staining in a patient with dry eye
After fluorescein sodium staining, the corneal epithelium exhibits diffuse punctate staining under cobalt blue light.
Lissamine Green Staining
This dye stains devitalized or degenerated cells and corneal or conjunctival epithelial cells deficient in mucin coverage. Being non-irritating, unlike rose bengal, lissamine green is more acceptable to patients and can provide diagnostic evidence for mucin-deficient dry eye.
Imaging and Other Auxiliary Examinations
Meibomian Gland Imaging
Using infrared imaging, the morphology of the meibomian glands can be visualized. This method evaluates gland structural changes or atrophy and provides objective information regarding gland morphology.
Conjunctival Impression Cytology
Following surface anesthesia, cellulose acetate membranes are used to collect samples from the superior temporal bulbar conjunctiva. The samples are then PAS-stained and analyzed for the density and morphology of goblet and epithelial cells. This examination has diagnostic value for mucin-deficient dry eye.
Diagnosis and Differential Diagnosis
Diagnostic Process
Clinical evaluation of dry eye should follow a sequence moving from non-invasive to invasive methods, from no contact to contact, and from local to systemic examination. Key diagnostic procedures include patient history inquiry, symptom assessment, slit lamp examination, and tear film homeostasis evaluation. Auxiliary examinations may assist in pinpointing the etiology and assessing the severity of dry eye.
Diagnostic Criteria
Patients reporting ocular symptoms such as dryness, foreign body sensation, burning, fatigue, discomfort, or visual fluctuations, and showing a BUT ≤5 seconds or Schirmer I test result (without anesthesia) ≤5 mm/5 min, meet the diagnostic criteria for dry eye.
Patients exhibiting dry eye symptoms, with 5 seconds < BUT ≤10 seconds or 5 mm/5 min < Schirmer I test result (without anesthesia) ≤10 mm/5 min, require positive fluorescein staining of the cornea and conjunctiva (≥5 spots) to confirm a diagnosis of dry eye.
Differential Diagnosis
Since many ocular surface conditions share symptoms with dry eye, and dry eye often coexists with other ocular diseases, thorough patient history taking and detailed physical examination are crucial for differential diagnosis. Common conditions that may be confused with dry eye include allergic conjunctivitis, trichiasis, conjunctivochalasis, and visual fatigue.
Treatment
The treatment goals for dry eye are to eliminate potential causes, alleviate symptoms, and protect visual function.
Ocular Surface Lubrication and Tear Secretion Enhancement
Artificial Tears
Artificial tears are the first-line therapy for dry eye and are suitable for all types of dry eye. Their primary functions are to lubricate the ocular surface and dilute soluble inflammatory mediators on the ocular surface. Artificial tears that replenish moisture often contain ingredients such as sodium hyaluronate, carboxymethylcellulose, and polyvinyl alcohol. Lipid-containing artificial tears or those modeled on lipid structures can supplement the lipid layer of the tear film, while mucin-like artificial tears enhance adhesion between the tear film and the cornea.
Eye Drops Promoting Tear Secretion
Currently, medications such as P2Y2 receptor agonists (e.g., diquafosol sodium) are used to stimulate mucin secretion. These drugs primarily facilitate mucin secretion by conjunctival epithelial cells but also have a mild effect on promoting the secretion of aqueous and lipid components of the tear film.
Anti-Inflammatory Therapy
Commonly used anti-inflammatory medications include corticosteroids and immunosuppressants, which are mainly employed to treat moderate to severe dry eye. Additionally, medications containing active ingredients such as epidermal growth factor, fibroblast growth factor, and vitamin A can promote epithelial proliferation and maintain the ocular surface microenvironment. Certain antibiotics, such as tetracyclines, azithromycin, and fusidic acid, not only have antimicrobial effects but also possess mild anti-inflammatory properties, making them a preferred choice for patients with meibomian gland dysfunction (MGD) or lid margin abnormalities.
Physical Therapy
Lid Hygiene
Proper lid margin hygiene is crucial for treating dry eye related to eyelid abnormalities, especially blepharitis. Effective lid cleaning reduces the accumulation of harmful lipids and eliminates pathogenic microorganisms such as Demodex mites.
Warm Compress and Steam Therapy
Localized heating helps to restore the fluidity of thickened meibum, facilitating its expulsion and improving or restoring meibomian gland function. For optimal results, it is recommended that the meibomian gland temperature reaches 40°C during warm compresses. Patients can use items like warm towels or heated eye masks. Professional ocular steam equipment available in healthcare facilities may further promote the flow and release of meibum through regular therapy.
Meibomian Gland Massage
This technique involves mechanically squeezing the meibomian glands to unclog blocked gland orifices and express abnormal meibum.
Other Approaches
For patients who do not respond well to the aforementioned treatments, alternative options such as punctal occlusion, humidification devices, or the use of scleral lenses may be considered. Patients with corneal epithelial damage may benefit from wearing corneal bandage lenses.
Surgical Treatment
Surgical options may be considered for patients with significantly reduced tear secretion, where conventional treatments prove ineffective and there is a risk of severe visual impairment. Surgical techniques include lid margin suturing, conjunctivochalasis correction, amniotic membrane transplantation, and salivary gland transplants (e.g., from the submandibular or labial glands).
Health Education and Psychological Counseling
Patients should be educated about the nature of dry eye, including its natural disease course and treatment goals. Promoting the adoption of healthy lifestyle habits is important. For patients experiencing psychological challenges due to dry eye, active communication and emotional reassurance should be provided, and psychological intervention by specialists may be arranged if necessary.