Marginal corneal degeneration, also known as Terrien marginal degeneration, is a bilateral condition characterized by peripheral corneal thinning and ectasia. The etiology remains unclear. In the early stages of the disease, the corneal epithelium, Descemet's membrane, and endothelial layer appear normal, while defects or disruptions are observed in Bowman's membrane, along with abundant deposits of acidic mucopolysaccharides in the stromal layer. It is currently believed to be associated with immune-mediated inflammation. The condition predominantly affects males, with a male-to-female ratio of 3:1, typically manifesting in young adulthood (ages 20–30). Progression is slow and the disease course is lengthy. Although it often affects both eyes, it may present asymmetrically or at different times, with varying progression between the two eyes.
Clinical Manifestations
Pain and photophobia are generally absent. Vision experiences a chronic, progressive decline. Thinning and ectasia of the peripheral cornea occur symmetrically in one or both eyes, most commonly in the superonasal quadrant. In some cases, thinning and ectasia involve both the upper and lower peripheral cornea. As the condition advances, the areas of thinning in the upper and lower regions may gradually merge to form circumferential peripheral thinning. The thickness of the thinned region is typically reduced to one-fourth to one-half of the normal corneal thickness, with the thinnest areas sometimes consisting only of epithelium and a protruding Descemet's membrane. In some cases, minor trauma can result in perforation, although spontaneous perforation is rare. Shallow new blood vessels are observed in the thinned areas, and lipid deposits may be present along the advancing edge of the lesion. Irregular myopic astigmatism due to corneal thinning and ectasia results in progressive vision loss that is uncorrectable.
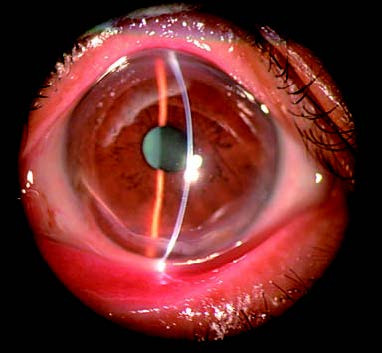
Figure 1 Marginal corneal degeneration
Thinning and ectasia are observed in the inferior peripheral cornea, causing forward protrusion of the inferior cornea.
Treatment
Medical therapy is ineffective, with surgical interventions being the primary approach. Early stages may benefit from corrective lenses to improve vision. For eyes with progressive corneal thinning and a risk of spontaneous perforation or rupture due to minor trauma, lamellar keratoplasty is an option. In cases with small corneal perforations, lamellar keratoplasty remains viable. For larger perforations or when ocular contents are exposed, penetrating keratoplasty is required.