Due to the unique pathophysiology of the cornea, immune-related inflammation of the cornea typically occurs in the peripheral cornea or the limbus. Among these, Mooren's ulcer is the most classic and representative type of immune keratitis.
Mooren's ulcer is a type of primary, chronic, and painful corneal ulcer, generally located in the peripheral cornea with progressive development. Its exact etiology remains unclear, but possible contributing factors include corneal trauma, surgery, or infections (such as helminthic infections, herpes zoster virus, syphilis, tuberculosis, hepatitis C, and salmonella).
Pathology and Immunological Features
The exact pathological mechanism is not well understood, but Mooren's ulcer is generally believed to be an autoimmune disease. In the affected areas, the conjunctiva displays extensive infiltration by plasma cells, lymphocytes, mast cells, and eosinophils. Serum immune complex levels are higher than those in the general population, and patients may exhibit a lymphocyte proliferation response to normal corneal stroma. Additionally, the ratio of systemic suppressor T lymphocytes to helper T lymphocytes in patients is reduced. These findings suggest that both cellular and humoral immunity are involved in the pathogenesis of the disease.
Clinical Manifestations
Mooren’s ulcer typically occurs in adults, with no significant difference in incidence between males and females. Most cases are unilateral, commonly affecting older adults, with relatively mild symptoms and slow progression. A smaller proportion of cases are bilateral, more common in younger individuals, with severe symptoms and rapid disease progression. Symptoms primarily include severe ocular pain, photophobia, tearing, and decreased vision.
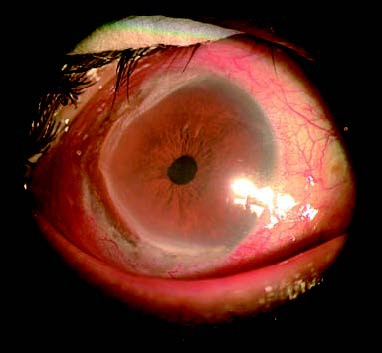
Figure 1 Mooren's ulcer
An ulcer is present in the peripheral cornea, spreading circumferentially along the limbus and infiltrating toward the central corneal region. The edge of the infiltrated area appears undermined and slightly elevated.
In the early stages of the disease, shallow stromal infiltration appears in the peripheral cornea, often located on the nasal or temporal side. This is followed by epithelial defects in the infiltrated areas, eventually resulting in ulceration. The ulcer progresses in a circumferential pattern along the limbus and the infiltration spreads toward the central cornea. The edges of the infiltrated areas appear undermined and slightly elevated, and the disease may ultimately affect the entire cornea. In rare cases, the ulcer may deepen, leading to corneal perforation. One characteristic feature of this condition is the lack of normal corneal tissue separating the ulcer from the limbus. However, the ulcer does not extend beyond the limbus to involve the sclera. As the ulcer progresses toward the central cornea, the epithelium at its peripheral edges may gradually heal, accompanied by ingrowth of new blood vessels and the formation of a peripheral fibrovascular membrane-like proliferation.
Before diagnosing Mooren's ulcer, systemic diseases that may cause peripheral corneal ulcers, such as rheumatoid arthritis or Wegener's granulomatosis, should be ruled out. Relevant laboratory tests are helpful in excluding these conditions.
Treatment
Treatment for this condition is quite challenging. Topical corticosteroids or collagenase inhibitors (e.g., 2% cysteine eye drops) may be used. Eyedrops containing 1%–2% cyclosporine or tacrolimus (FK506) have shown some efficacy. Topical antibiotic eye drops and ointments are used to prevent secondary infections. Supplementation with vitamin-based medications is also necessary. For severe cases or in bilateral involvement, systemic immunosuppressants such as cyclophosphamide, methotrexate, and cyclosporine have shown some effectiveness.
Surgical treatment is often required for this condition. When the lesion is confined to the peripheral cornea and is relatively superficial, superficial keratectomy combined with conjunctival resection in adjacent areas can help control the disease. For larger lesions or those involving the pupillary zone, crescent-shaped, ring-shaped, or full-thickness lamellar keratoplasty may be considered, depending on the extent of the disease. In cases of deep ulcers with a risk of perforation or existing corneal perforation, penetrating keratoplasty may be performed. Postoperatively, continued medical therapy is necessary, with cyclosporine or tacrolimus showing some efficacy in preventing recurrence.