Subconjunctival hemorrhage occurs due to ruptured blood vessels beneath the bulbar conjunctiva or increased vascular permeability. Because of the loose structure of the subconjunctival tissue, the blood tends to pool and form sheet-like areas after hemorrhage. Strictly speaking, subconjunctival hemorrhage is a symptom rather than a specific disease, and identifying a definitive cause is often challenging. It most commonly occurs unilaterally and can affect individuals of any age. Occasionally, a history of violent coughing, vomiting, or other events may precede the hemorrhage. Other potentially related medical histories include trauma (ocular or head injuries), conjunctival inflammation, hypertension, arteriosclerosis, nephritis, hematologic disorders (such as leukemia or hemophilia), or certain infectious diseases (such as typhoid fever).
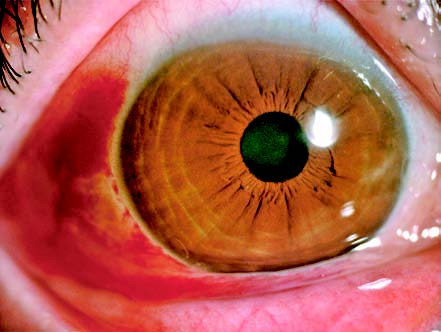
Figure 1 Subconjunctival hemorrhage
Clinical Manifestations
Initially, the hemorrhage appears bright red but gradually changes to a brownish hue over time. It typically resolves spontaneously within 7 to 12 days. In cases where the volume of blood is significant, the hemorrhage may spread circumferentially around the globe. Recurrent episodes may warrant a thorough investigation for systemic diseases.
Treatment
The primary focus lies in identifying the underlying cause of the hemorrhage and treating the associated condition. In the early stages, localized cold compresses may be applied, followed by warm compresses after two days, performed twice daily, which may aid in the absorption of the hemorrhage. Providing reassurance and clear explanations to the patient can help alleviate concerns.