Under normal conditions, bacteria are present within the conjunctival sac, with approximately 90% of individuals carrying bacteria and about 35% harboring more than one bacterial strain. These normal flora primarily include Staphylococcus epidermidis (>60%), Staphylococcus aureus, and Pseudomonas aeruginosa. These bacteria can reduce the invasion of other pathogens by releasing antibiotic-like substances and metabolic products. Infections may occur when the pathogenic bacteria overpower the host's defense mechanisms or when the host's defenses are compromised, such as in cases of dry eye or prolonged use of corticosteroids. Bacterial conjunctivitis (bacterial conjunctivitis) should be considered when patients exhibit varying degrees of conjunctival hyperemia and purulent, mucoid, or mucopurulent discharge in the conjunctival sac. Based on the speed of onset, bacterial conjunctivitis can be classified into hyperacute (within 24 hours), acute or subacute (from several hours to several days), and chronic (lasting several days to weeks). Based on the severity of the condition, it can be categorized as mild, moderate, or severe. Acute conjunctivitis is generally self-limiting, with a course of approximately two weeks, and effective local therapy can reduce the severity of inflammation and shorten the duration of the disease. Full recovery is typically achieved within a few days after treatment with appropriate antibiotics. Chronic conjunctivitis is not self-limiting and is more challenging to treat.
Etiology
Common pathogenic bacteria are listed in Table 1.
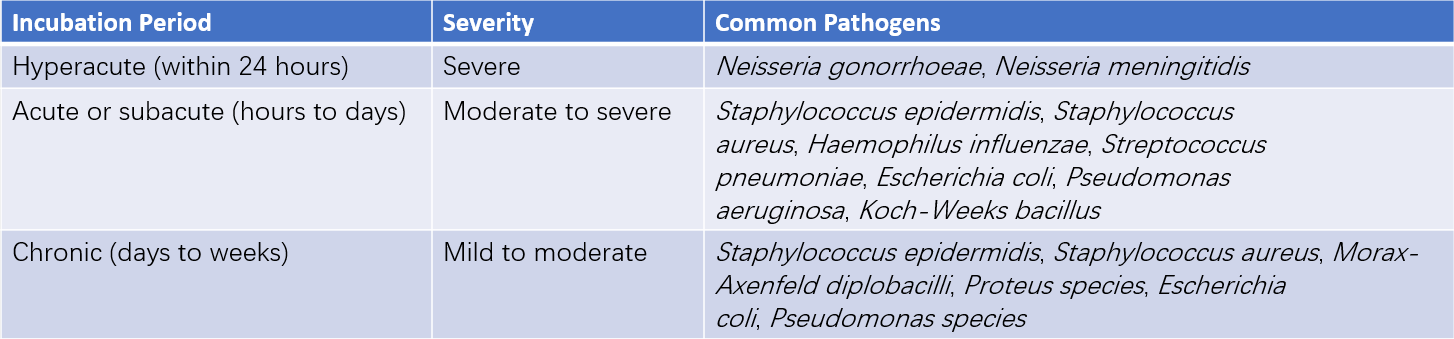
Table 1 Common pathogens in various types of bacterial conjunctivitis
Clinical Manifestations
Acute papillary conjunctivitis accompanied by catarrhal or mucopurulent exudate is a characteristic manifestation of most bacterial conjunctivitis cases. The condition typically begins in one eye and spreads to the other through hand contact. Patients may experience ocular irritation and conjunctival hyperemia. Sticky secretions may accumulate along the eyelid margins upon waking, with the initial discharge being serous and later becoming mucoid or purulent as the disease progresses. Occasional eyelid edema may occur. Vision is generally unaffected, but epithelial haze resulting from corneal involvement may lead to visual impairment. The severity of papillary proliferation and follicular formation in bacterial conjunctivitis depends on the virulence and invasiveness of the causative bacteria.
Hyperacute Bacterial Conjunctivitis
This form is caused by bacteria of the Neisseria genus (N. gonorrhoeae or N. meningitidis). Its defining features include a short incubation period (10 hours to 2–3 days) and rapid progression. Conjunctival hyperemia and edema are accompanied by profuse purulent secretions. Corneal opacity and infiltration, as well as peripheral or central corneal ulcers, develop in 15–40% of cases, posing a significant threat to vision. Corneal perforation may occur within days if treatment is delayed. Adult gonococcal conjunctivitis often results from genital-eye contact, while neonates typically acquire the infection during delivery from mothers with gonococcal vaginitis. Neonatal infection has an incidence of approximately 0.04%. Neisseria meningitidis conjunctivitis commonly arises from hematogenous dissemination but can also be transmitted through respiratory secretions. It is more prevalent in children, often involves both eyes, has an incubation period of only a few hours to one day, and presents similarly to gonococcal conjunctivitis. Severe cases may progress to purulent meningitis, which can be life-threatening. The two conditions can be difficult to distinguish clinically, and both pathogens can cause systemic dissemination, including septicemia. Specific diagnosis requires bacterial culture and carbohydrate fermentation testing. The emergence of penicillin-resistant Neisseria strains underscores the importance of conducting antibiotic susceptibility testing.
Neonatal Gonococcal Conjunctivitis
The incubation period is 2–5 days. Cases involving infection during delivery present within seven days of birth, while those occurring later are typically postpartum infections. Both eyes are frequently affected. Symptoms include photophobia, tearing, and severe conjunctival edema, which in extreme cases may protrude through the palpebral fissure. Pseudomembrane formation may occur, and secretions rapidly transition from serous to purulent, with copious amounts of pus continuously discharged, earning the condition the name "blennorrhea." Preauricular lymphadenopathy with tenderness is often observed. Severe cases may result in corneal ulceration or endophthalmitis. Concurrent purulent infections in other locations, such as arthritis, meningitis, pneumonia, or septicemia, may occur in affected infants.
Acute or Subacute Bacterial Conjunctivitis
Also referred to as "acute catarrhal conjunctivitis" or "pink eye," this form is highly contagious and more prevalent during the spring and autumn seasons. It may occur sporadically or in outbreaks in communal settings such as schools and factories. The condition has a sudden onset, with an incubation period of 1–3 days. Both eyes may become affected simultaneously or within 1–2 days of each other. Inflammation is most severe on the third or fourth day of illness and gradually subsides. The disease typically resolves within three weeks. Common causative bacteria include Staphylococcus epidermidis, Staphylococcus aureus, Haemophilus influenzae, and Streptococcus pneumoniae, listed in descending order of prevalence.
Staphylococcus epidermidis and Staphylococcus aureus Conjunctivitis
Blepharitis often accompanies this type. It can occur at any age. Patients may experience difficulty opening their eyes in the morning due to dried mucopurulent secretions crusting the eyelids shut. Corneal involvement is rare.
Streptococcus pneumoniae Conjunctivitis
This form is self-limiting and more common in children than adults. Symptoms such as conjunctival hyperemia and mucopurulent discharge peak within 2–3 days after an incubation period of approximately two days. Subconjunctival hemorrhages may be seen in the upper palpebral and fornix conjunctiva, along with chemosis of the bulbar conjunctiva. Upper respiratory tract symptoms may accompany the condition, though pneumonia is rare.
Haemophilus Influenzae
This is the most common pathogen causing bacterial conjunctivitis in children. The incubation period is approximately 24 hours. Clinical manifestations include conjunctival congestion, edema, subconjunctival hemorrhage, and purulent or mucopurulent discharge. Symptoms peak around 3–4 days and resolve within 7–10 days after initiating antibiotic treatment. Without treatment, recurrence is possible. Infection in children can lead to periorbital cellulitis, with some patients also exhibiting systemic symptoms such as fever and malaise.
Others
Conjunctivitis caused by Corynebacterium diphtheriae may present as acute membranous or pseudomembranous conjunctivitis. In early stages, symptoms include redness, swelling, heat, and pain in the eyelid, often accompanied by preauricular lymphadenopathy. Severe cases may involve the formation of grayish-yellow membranes or pseudomembranes on the surface of the bulbar conjunctiva, which may leave scars upon necrotic detachment. Corneal ulcers are rare but, if they occur, are prone to perforation. Diphtheria toxin may result in paralysis of extraocular muscles and accommodation. Common complications include dry eye, symblepharon, trichiasis, and entropion. This condition is highly contagious and requires systemic antibiotic therapy.
Chronic Bacterial Conjunctivitis
This form may evolve from acute conjunctivitis or may result from infection with low-virulence pathogens. It is commonly observed in individuals with nasolacrimal duct obstruction, chronic dacryocystitis, chronic blepharitis, or meibomian gland dysfunction. Common causative pathogens include Staphylococcus epidermidis, Staphylococcus aureus, and Moraxella species.
Chronic conjunctivitis typically progresses slowly and lasts for an extended period. It can occur unilaterally or bilaterally. Symptoms vary widely, with common complaints including itching, burning, dryness, stabbing pain in the eyes, and visual fatigue. Conjunctival involvement is usually mild, presenting as slight hyperemia, thickening of the palpebral conjunctiva, and papillary hyperplasia. Secretions are generally mucoid or appear as white foam-like discharge. Moraxella species can cause angular conjunctivitis, which may be associated with crusts and ulcers on the skin near the outer canthus, as well as papillary and follicular hyperplasia in the palpebral conjunctiva. Cases associated with Staphylococcus aureus are often accompanied by ulcerative blepharitis or peripheral corneal infiltration.
Diagnosis
Diagnosis is established based on clinical presentation and examination of secretions or conjunctival scrapings. Gram and Giemsa staining of conjunctival scrapings and discharge may reveal numerous polymorphonuclear leukocytes and bacteria under a microscope. For confirmation of the causative pathogen and to guide treatment, bacterial culture and antibiotic susceptibility testing are recommended in cases with abundant purulent discharge, severe conjunctivitis in children and infants, or treatment-resistant cases. Blood cultures are warranted in patients with systemic symptoms.
Treatment
Treatment involves addressing the underlying cause and conducting anti-infective therapy. While waiting for laboratory results, broad-spectrum antibiotics are used locally. Once the specific pathogen is identified, sensitive antibiotics are administered. Depending on the severity of the condition, methods such as conjunctival sac irrigation, local application of medication, systemic treatment, or combined therapies are employed. It is important to avoid eye patching, although wearing sunglasses can help reduce light-induced irritation. For hyperacute bacterial conjunctivitis, treatment begins immediately after diagnostic specimens are collected to minimize the risk of corneal and systemic infections. A combination of local and systemic therapies is used. Acute or subacute bacterial conjunctivitis in adults is generally treated with eye drops, while children typically receive ointments. The treatment principles for chronic bacterial conjunctivitis are similar to those for the acute form, but longer-term therapy is often required.
In cases where different types of conjunctivitis involve the cornea, treatment should follow the principles for keratitis.
Local Therapy
For cases with abundant ocular discharge, non-irritating solutions such as 3% boric acid or normal saline can be used to irrigate the conjunctival sac.
Effective antibiotic eye drops and ointments are applied locally. During the acute phase, these are administered every 1–2 hours. Commonly used broad-spectrum antibiotics include aminoglycosides or fluoroquinolones, such as 0.3% tobramycin, 1% azithromycin, 0.3% ofloxacin, 0.5% moxifloxacin, 0.3% gatifloxacin, and 0.3%–0.5% levofloxacin in the form of eye drops or ointments. For conjunctivitis caused by resistant Staphylococcus species, vancomycin (5 mg/mL) eye drops may be used. Chronic Staphylococcus-related conjunctivitis generally responds well to bacitracin and erythromycin, and astringents such as 0.25% zinc sulfate eye drops can also be applied as needed.
Systemic Therapy
For Neisseria-associated conjunctivitis, systemic antibiotics must be administered promptly and in sufficient doses, either through intramuscular injection or intravenous infusion. In adults with gonococcal conjunctivitis where the cornea is unaffected, a single large dose of penicillin or ceftriaxone sodium (1 g) is sufficient. If the cornea is involved, the dosage is increased to 1–2 g/day, continued for five days. For patients allergic to penicillin, spectinomycin (2 g/day intramuscularly) can serve as an alternative. Additional treatments include single doses of 1 g azithromycin or 100 mg doxycycline twice daily for seven days, or fluoroquinolones such as 0.5 g ciprofloxacin or 0.4 g ofloxacin, both administered twice daily for five days.
Neonates receive 100,000 U/(kg·d) of penicillin G through intravenous infusion or four divided intramuscular doses daily for seven days. Alternatives include 0.125 g ceftriaxone (intramuscularly) or 25 mg/kg cefotaxime (intravenously or intramuscularly) administered every 8 or 12 hours for seven days.
Conjunctivitis caused by Neisseria meningitidis, which may progress to meningococcal septicemia, requires systemic treatment. Penicillin is given as an intravenous or intramuscular injection, with chloramphenicol provided as an alternative for penicillin-allergic patients. Individuals with a history of exposure are given prophylactic treatment, such as rifampin taken orally twice daily for two days. The recommended dose is 600 mg/day for adults and 10 mg/(kg·d) for children.
For acute bacterial conjunctivitis caused by Haemophilus influenzae, or when associated with pharyngitis or acute suppurative otitis media, local treatment is accompanied by systemic administration of cephalosporin antibiotics or rifampin.
In refractory cases of chronic conjunctivitis and in patients with rosacea, doxycycline (100 mg) is administered orally once or twice daily until symptoms resolve.
Prevention
Maintaining strict personal and communal hygiene is essential. Frequent handwashing and face washing are encouraged, avoiding the use of hands or clothing to rub the eyes.
During the acute phase, patients need to be isolated to prevent transmission and curb outbreaks. When one eye is affected, measures are taken to protect the unaffected eye from infection.
Thorough disinfection of the patient’s personal items, such as towels and handkerchiefs, and medical instruments that come into contact with the patient is necessary.
Healthcare professionals must wash and disinfect their hands after coming into contact with patients to prevent cross-infection. Protective eyewear may be required when appropriate.
Routine prophylactic measures for neonates immediately after birth consist of administering 1% silver nitrate eye drops or applying 0.5% tetracycline eye ointment once to prevent gonococcal or chlamydial conjunctivitis.