Lacrimal duct obstruction is a common ophthalmological condition that frequently occurs at the junction of the canaliculus, lacrimal sac, and nasolacrimal duct, as well as at the distal opening of the nasolacrimal duct. The proximal portion of the lacrimal drainage system, including the puncta, canaliculi, and common canaliculus, is narrow and superficially located, making it susceptible to inflammation and trauma. The distal opening of the nasolacrimal duct is an anatomically constricted area and is prone to obstruction due to nasal pathology. In addition, reduced or absent tear pump function can result in functional epiphora.
Etiology
Punctal Abnormalities
Punctal eversion prevents contact with the tear lake and is often seen in elderly patients with eyelid laxity or ectropion. Other abnormalities include punctal stenosis, atresia, or absence.
Lacrimal Drainage Abnormalities
Obstruction or stenosis of the canaliculi may arise from inflammation, exudation, or secondary scarring of the canalicular mucosa. Obstruction or stenosis of the nasolacrimal duct may stem from congenital atresia, inflammation, tumors, dacryoliths, trauma, or foreign bodies that impede tear outflow. Nasal abnormalities can also result in nasolacrimal duct obstruction. In infants, nasolacrimal duct obstruction is often caused by underdevelopment of the distal nasolacrimal duct or the persistence of a membranous fold (Hasner's valve) at birth, leading to infantile epiphora. In middle-aged and older adults, organic lesions are a more common cause.
Reduced Tear Pump Function in the Elderly
Some elderly individuals, despite having no obvious lacrimal duct obstruction, may experience tear outflow impairment due to laxity of the orbicularis oculi muscle, resulting in diminished or absent tear pump function and causing functional epiphora.
Clinical Presentation
The primary symptom of lacrimal duct obstruction or stenosis is epiphora. Infantile epiphora can affect one or both eyes, and secondary infection of the lacrimal sac may result in mucopurulent discharge, leading to neonatal dacryocystitis. In middle-aged and older adults, epiphora can cause discomfort, and prolonged exposure to excessive tears may result in chronic irritative conjunctivitis, irritant dermatitis of the lower eyelid, and cheek skin. Repeated wiping of tears over time can lead to laxity and eventual ectropion of the lower eyelid, further exacerbating the epiphora.
Diagnostic Methods
Evaluation includes identifying punctal eversion or obstruction, as well as checking for redness, swelling, tenderness, or fistulas in the lacrimal sac region. Pressing on the lacrimal sac may reveal discharge from the puncta. Determining the site of obstruction is crucial for treatment planning, and the following diagnostic methods are commonly used:
Dye Test
A 2% fluorescein sodium solution is instilled into the conjunctival sacs of both eyes. After 5 minutes, the degree of fluorescence in the tear film of each eye is compared. Retention of fluorescein in one eye suggests partial lacrimal duct obstruction or stenosis. Alternatively, after instilling fluorescein, a wet cotton swab is applied to the inferior nasal meatus after 5 minutes. The presence of green-yellow staining on the swab indicates patency or incomplete obstruction of the lacrimal duct.
Lacrimal Irrigation
This technique often helps identify the location of an obstruction. A blunt-tipped cannula is used to inject saline into the lacrimal system through the puncta, and the flow of the solution is observed:
- Unobstructed flow: The saline passes freely into the nasal cavity or throat, indicating normal patency.
- Complete reflux from the original canaliculus: Indicates canalicular obstruction.
- Reflux through the opposite punctum: Saline injected into the upper punctum flows back from the lower punctum (or vice versa), indicating obstruction in the common canaliculus, lacrimal sac, or nasolacrimal duct.
- Partial reflux with resistance: Some saline flows back from the punctum, while some enters the nasal cavity, suggesting nasolacrimal duct stenosis.
- Reflux with mucopurulent discharge: Indicates nasolacrimal duct obstruction complicated by chronic dacryocystitis.
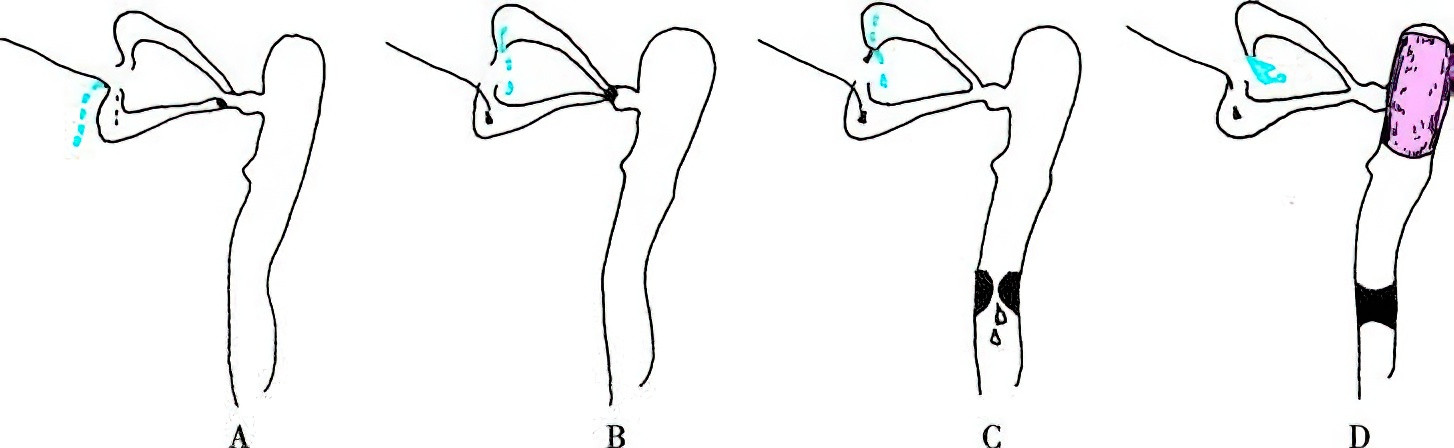
Figure 1 Diagram illustrating lacrimal irrigation
A. Canalicular Obstruction: The irrigation fluid fully refluxes from the original point of entry.
B. Common Canalicular Obstruction: Irrigation fluid refluxes (fluid introduced into the lower canaliculus refluxes from the upper canaliculus, and vice versa).
C. Nasolacrimal Duct Stenosis: Most of the irrigation fluid refluxes.
D. Chronic Dacryocystitis: Irrigation fluid refluxes with purulent discharge.
Lacrimal Probing
Diagnostic lacrimal probing helps localize obstruction in the punctum, canaliculus, or lacrimal sac. Therapeutic probing is primarily used for infantile lacrimal duct obstruction. In adults with nasolacrimal duct obstruction, probing generally does not provide definitive treatment.
Imaging Studies
Imaging modalities such as X-ray dacryocystography with iodized oil or CT dacryocystography can reveal the size of the lacrimal sac and the site and degree of lacrimal duct stenosis or obstruction. Endoscopic examination of the lacrimal ducts also provides direct visualization.
Treatment
Infantile Nasolacrimal Duct Obstruction or Stenosis
The preferred approach is local massage. The technique involves applying the index finger to the lacrimal sac area and performing regular massage and compression 3 to 4 times daily for several weeks to facilitate the opening of the distal nasolacrimal duct. In cases where dacryocystitis is present, cleaning the area after compression and the application of antibiotic eye drops can help reduce inflammation and prevent its spread. Most infants naturally recover as the nasolacrimal duct develops and the distal end opens on its own, or the pressure from massage breaks through Hasner's valve, leading to resolution. If conservative treatment is ineffective, lacrimal probing may be considered.
Punctal Stenosis, Occlusion, or Absence
Treatment for punctal stenosis may involve the use of punctal dilators or lacrimal probing. In cases of punctal occlusion or absence, punctoplasty can be performed. Placement of a silicone tube postoperatively helps counteract scar contraction during tissue healing, preventing recurrent stenosis or occlusion. For complete absence of the puncta and canaliculi, conjunctivodacryocystorhinostomy may be performed.
Punctal Malposition
For punctal eversion, treatment may involve excising an elliptical piece of conjunctiva and subconjunctival tissue parallel to the eyelid margin below the punctum to reposition it. In cases of eyelid laxity or ectropion, corrective surgery for eyelid laxity or ectropion may be performed.
Canalicular Stenosis or Obstruction
Canalicular stenosis can be managed with lacrimal intubation, leaving a silicone tube in place within the lacrimal duct for 3 to 6 months. Canalicular obstruction may be treated using direct visualization under a lacrimal endoscope, employing techniques such as laser treatment, microdrilling, or ring knife incisions to restore patency of the canaliculi or common canaliculus. Silicone intubation is typically maintained for 3 to 6 months postoperatively.
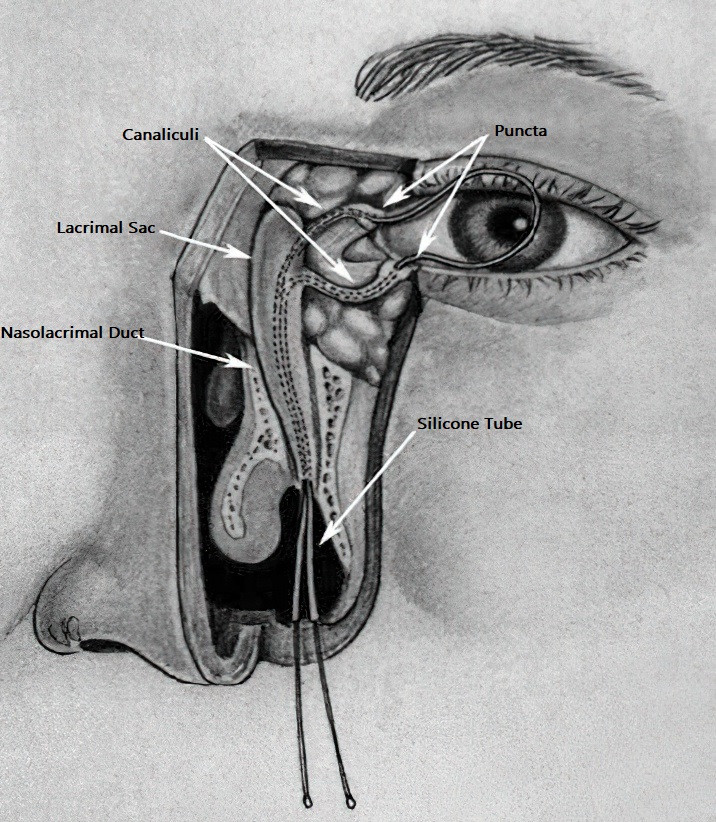
Figure 2 Diagram of annular lacrimal intubation
Nasolacrimal Duct Stenosis or Obstruction
For nasolacrimal duct stenosis, lacrimal probing combined with intubation may be employed. In cases of nasolacrimal duct obstruction, external dacryocystorhinostomy (DCR) via a percutaneous approach or endoscopic dacryocystorhinostomy via the nasal cavity may be performed.