Glomus jugular tumor, also known as jugular paraganglioma, is the most common tumor in the jugular foramen region. It originates from the paraganglionic cells of the chemoreceptor in the jugular bulb. The tumor is highly vascular, slow-growing, but aggressive. It often grows outward from the jugular bulb, invading the middle ear, mastoid process, facial nerve, petrous part of the temporal bone, and internal carotid artery. Unlike visceral paragangliomas, head and neck paragangliomas are less likely to exhibit neuroendocrine activity.
Clinical Manifestations
This condition is more commonly observed in young and middle-aged females, with a male-to-female ratio of approximately 1:5. The disease progression is typically slow, and early stages may be asymptomatic. Pulsatile tinnitus on the affected side is the most common clinical symptom. When the tumor extends into the external auditory canal, bloody otorrhea may occur. If it invades the tympanic cavity, conductive hearing loss may result, and further invasion into the inner ear may cause mixed or sensorineural hearing loss, vertigo, and other symptoms. Facial nerve involvement by the tumor may lead to varying degrees of peripheral facial paralysis on the affected side. Tumor involvement of cranial nerves IX, X, XI, or XII can result in symptoms such as choking, hoarseness, paralysis of the sternocleidomastoid and trapezius muscles, or tongue muscle atrophy. Intracranial extension may cause symptoms of increased intracranial pressure, such as headache, nausea, and vomiting, as well as other signs of cranial nerve impairment.
During otoscopic examination, a pulsatile dark red mass is sometimes visible through the tympanic membrane. Larger tumors may cause bulging of the tympanic membrane or perforation, exposing part of the pulsatile red polypoid tumor, which bleeds easily upon contact.
Diagnosis
The condition should be considered in patients with a history of long-standing pulsatile tinnitus, hearing loss, and a sensation of ear fullness or pressure. On physical examination, a deep red tympanic membrane, along with bloody otorrhea or granulomatous tissue in the external auditory canal that bleeds easily upon contact, are key indicators.
CT imaging of the temporal bone often shows bone destruction around the jugular foramen with blurred margins. Irregular soft tissue opacities are frequently noted in the middle ear and mastoid, along with destruction of mastoid air cells, the bony labyrinth, and structures surrounding the internal carotid artery. On MRI, the tumor appears isointense or hypointense on T1-weighted images and isointense to hyperintense on T2-weighted images, with marked enhancement on contrast imaging. The "salt-and-pepper" appearance, attributed to flow voids in the vascular tumor, is a characteristic feature. Digital subtraction angiography (DSA) provides details on the tumor's blood supply, its relationship with the internal carotid artery, and sigmoid sinus–internal jugular venous drainage on the affected side. Preoperative embolization of the feeding vessels may be performed to reduce blood loss during surgery. If sacrificing the internal carotid artery is a possibility, a balloon occlusion test is necessary.

Figure 1 Axial CT features of a glomus jugular tumor of the temporal bone
Bone destruction and lytic changes are visible in the left jugular foramen region. The tumor invades the mastoid, external auditory canal, and tympanic cavity.
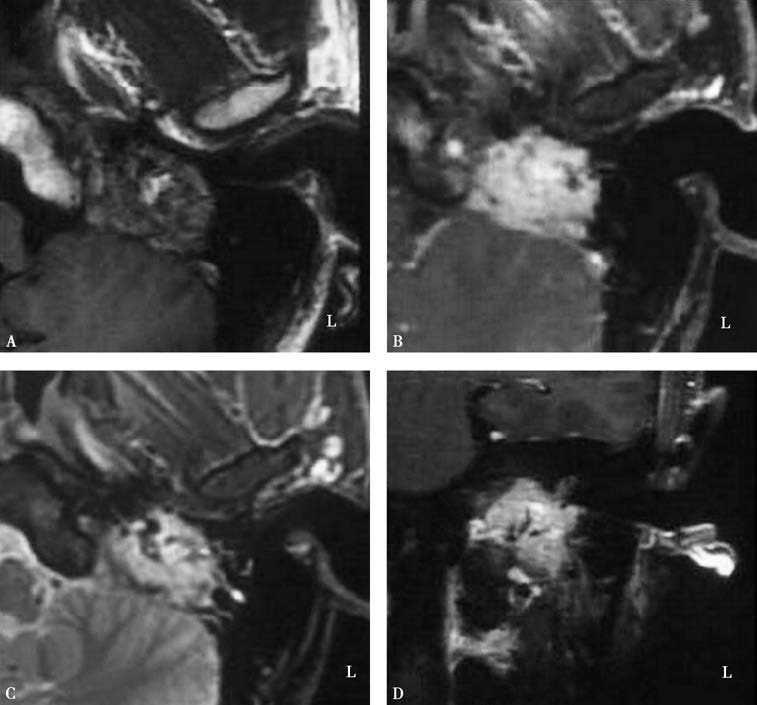
Figure 2 MRI features of a glomus jugular tumor
A. Axial view showing a tumor in the left jugular foramen region with isointense signals on T1-weighted imaging (T1WI).
B. Axial view with hyperintense signals on T2-weighted imaging (T2WI).
C. Axial view showing significant tumor enhancement with the characteristic "salt-and-pepper" appearance.
D. Coronal view showing significant tumor enhancement with the characteristic "salt-and-pepper" appearance.
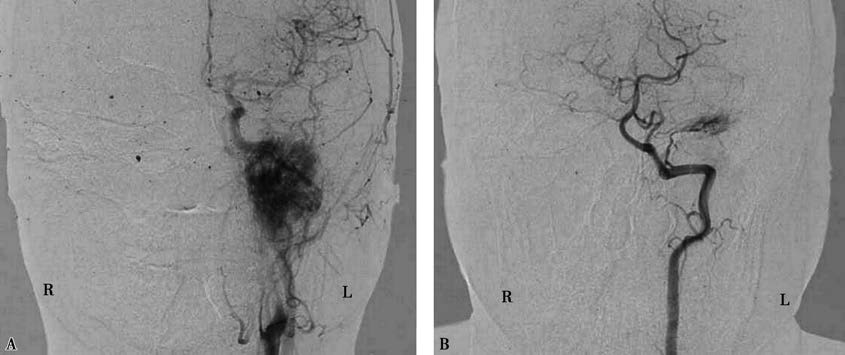
Figure 3 Angiographic findings of a glomus jugular tumor
A. Coronal view of the left external carotid artery angiogram showing distinct visualization of the tumor.
B. Coronal view of the left vertebral artery angiogram revealing a small branch supplying the tumor.
Tumor Classification
The clinical classification often follows the system proposed by Professor Fisch:
- Class A: Tumors confined to the tympanic cavity.
- Class B: Tumors originating from the lower tympanic cavity, involving the tympanic cavity and mastoid.
- Class C: Tumors causing bone destruction around the jugular bulb, invading the infralabyrinthine area and petrous apex, with varying degrees of involvement of the internal carotid artery.
- Class D: Tumors extending intracranially.
Treatment
Management of glomus jugular tumors primarily involves surgical resection and radiotherapy (including stereotactic radiosurgery).
Surgical Resection
Complete tumor removal is the preferred treatment, while preserving the integrity of major blood vessels and cranial nerves as much as possible. The surgical approach is selected based on tumor classification:
- For Class A lesions, surgery can be performed by tympanotomy via the ear canal.
- Class B tumors can often be managed with an open mastoidectomy.
- For Class C and D cases, tumor removal typically requires an infratemporal fossa type A approach. Intracranial invasion necessitates a collaborative effort between otolaryngologists and neurosurgeons.
Radiotherapy
In cases where extensive tumor involvement prevents complete resection, for recurrent tumors after surgery, or for patients in poor overall health who are unable to undergo surgery, radiotherapy (e.g., stereotactic radiosurgery) can be utilized. It may help control tumor growth and alleviate symptoms to some extent.