Malignant tumors of the larynx are among the most common malignancies of the head and neck region, ranking second in incidence among respiratory tract tumors, following lung cancer. They are more frequently observed in men than in women, with squamous cell carcinoma accounting for over 95% of cases. Other less common pathological types include verrucous carcinoma, papillary squamous carcinoma, basaloid squamous carcinoma, spindle cell carcinoma, adenosquamous carcinoma, mucoepidermoid carcinoma, adenoid cystic carcinoma, chondrosarcoma, malignant lymphoma, atypical carcinoid, and malignant melanoma.
Laryngeal Carcinoma
Epidemiology
Laryngeal carcinoma, commonly referring to laryngeal squamous cell carcinoma, is most frequently seen in men aged 50 to 70. However, in recent years, the age of onset has been decreasing due to the growing prevalence of smoking at younger ages. The increased number of women who smoke has also contributed to a rise in the disease's prevalence among females. Laryngeal carcinoma exhibits distinct geographical variations, with higher incidences observed in Central and Eastern Europe, Cuba, Spain, and Uruguay.
Etiology
The exact cause remains unclear, but it is generally believed to result from the combined effects of multiple carcinogenic factors.
Smoking and Alcohol Consumption
Smoking is known to trigger respiratory tract tumors, as tobacco can slow or halt ciliary movement in the airway, cause mucosal congestion and edema, and lead to epithelial hyperplasia and squamous metaplasia, creating a significant foundation for carcinogenesis. The majority of laryngeal carcinoma cases are associated with a long history of smoking, with the incidence positively correlated with the daily quantity and cumulative duration of smoking. Prolonged exposure to secondhand smoke can also lead to carcinogenesis. Alcohol consumption significantly increases the risk of supraglottic carcinoma, and the combination of smoking and drinking can produce a synergistic effect, exponentially raising the risk.
Precancerous Lesions
Precancerous lesions with a high malignant transformation potential include laryngeal keratosis (e.g., leukoplakia and pachydermia), adult-type hypertrophic laryngitis, and adult-onset laryngeal papillomas.
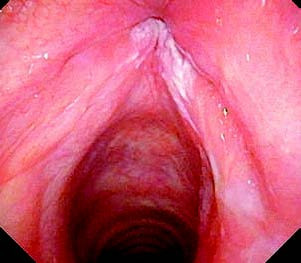
Figure 1 Laryngeal leukoplakia
Air Pollution and Occupational Exposure
High levels of air pollution in urban areas are associated with an increased incidence of laryngeal carcinoma. City residents are more prone to the disease than people living in rural areas. Prolonged inhalation of sulfur dioxide, chromium, arsenic, or exposure to polycyclic aromatic hydrocarbons, asbestos, mustard gas, and other carcinogens also elevates the risk of developing laryngeal carcinoma.
Other Factors
Contributing factors may include viral infections, nutritional deficiencies, hormonal imbalances, genetic susceptibility, activation of oncogenes, and inactivation of tumor suppressor genes.
Pathology
Laryngeal carcinoma can be classified as either primary or secondary. Primary laryngeal carcinoma accounts for over 95% of cases and is predominantly squamous cell carcinoma. Depending on the site of origin, primary laryngeal carcinoma is categorized as supraglottic carcinoma, glottic carcinoma, or subglottic carcinoma. Glottic carcinoma is the most common and accounts for approximately 60% of cases, followed by supraglottic carcinoma (30%), while subglottic carcinoma is rare. Secondary laryngeal carcinoma is uncommon and usually results from the spread of tumors originating in the thyroid, hypopharynx, base of the tongue, upper segments of the trachea, or esophagus. Metastatic laryngeal carcinoma from distant sites is exceedingly rare.

Figure 2 Glottic carcinoma
Macroscopically, laryngeal carcinoma can be divided into four types:
Ulcerative-Infiltrative Type
The tumor tissue mildly protrudes to the mucosal surface, with deeply infiltrating ulceration visible. The margins are often irregular, and the boundaries are unclear.
Exophytic (Papillary) Type
The tumor grows outward in a cauliflower-like pattern with clear boundaries; ulcer formation is generally absent.
Nodular or Mass-Forming Type
The tumor presents as an irregular or spherical elevation, often with an intact capsule and relatively clear boundaries. Ulceration is rare in this type.
Mixed Type
This type exhibits features of both ulcerative and exophytic patterns, with an irregular surface and often deep ulcerations.
Tumor Spread and Metastasis
In terms of embryological development, the supraglottic region originates from the oropharyngeal embryonic primordium, while the glottic and subglottic regions arise from the laryngotracheal embryonic primordium. This leads to differences in the fibrous fascia structures and lymphatic drainage of these areas, with the bilateral glottic regions forming relatively independent compartments. These differences in embryological origins form the oncological basis for partial laryngectomy procedures.
The spread and metastasis of laryngeal carcinoma are closely related to the primary tumor's location, degree of differentiation, and size. The main pathways of spread include:
Direct Spread
Supraglottic carcinoma can spread through vascular and neural foramina on the epiglottic cartilage or by destroying the epiglottic cartilage to invade the lingual surface. Horizontally, it may extend to the pre-epiglottic space and epiglottic vallecula. Superiorly, it may invade the tongue base, while peripherally it may extend to the aryepiglottic fold, ventricular fold, laryngeal ventricle, or even the vocal cord.
Glottic carcinomas often originate at the anterior-middle third junction of the vocal cords and may cross the anterior commissure to the contralateral vocal cord. Posteriorly, they can invade the cricoarytenoid joint, impairing vocal cord mobility, and can extend superiorly to involve the laryngeal ventricle and ventricular fold or inferiorly to the subglottic region. Deep invasion into the paraglottic space and destruction of the thyroid cartilage or cricothyroid membrane, leading to extralaryngeal extension, may occur in advanced stages.
Subglottic carcinomas can spread inferiorly to invade the trachea, superiorly to the vocal cords, anteriorly through the cricothyroid membrane to the prevertebral muscle layer, laterally to the thyroid gland, and posteriorly to the anterior wall of the esophagus.
Cervical Lymph Node Metastasis
Cervical lymph node metastasis is influenced by the tumor’s primary location, stage, degree of differentiation, and the patient’s immune status. Advanced-stage tumors, primary sites with rich lymphatic vasculature, poorly differentiated tumors, and patients with compromised immunity have higher rates of cervical metastasis.
The cervical metastasis of laryngeal carcinoma frequently involves the upper deep cervical lymph nodes, followed by the middle and lower groups. Lymphatic vessels are abundant in the supraglottic region, making lymphatic metastasis from supraglottic carcinoma more common.
Glottic carcinoma, in contrast, has limited lymphatic drainage due to the restriction of the conus elasticus, resulting in a lower incidence of lymphatic metastasis. Subglottic carcinoma or glottic carcinoma with subglottic invasion may metastasize to prelaryngeal lymph nodes and paratracheal lymph nodes. The latter is closely associated with local recurrence at the tracheostomy site. The presence or absence of cervical lymph node metastasis significantly affects the prognosis of patients with laryngeal carcinoma.
Hematogenous Metastasis
Hematogenous metastasis of laryngeal carcinoma is rare and typically occurs in late stages of the disease. The most common metastatic site is the lungs, followed by the liver, bone, and kidneys.
Clinical Manifestations
The primary symptoms of laryngeal carcinoma include hoarseness, a foreign body sensation in the throat, swallowing discomfort, breathing difficulties, cervical lymphadenopathy, and other symptoms such as cough, blood-streaked sputum, halitosis, throat pain, and choking.
Supraglottic Carcinoma
Early symptoms are often nonspecific, including a foreign body sensation in the throat, swallowing discomfort, halitosis, throat pain, blood-streaked sputum, or choking. Hoarseness may develop when the tumor involves the vocal cords. Larger tumors may obstruct the laryngeal cavity, leading to breathing or swallowing difficulties. Persistent throat complaints in individuals over middle age warrant careful consideration.
Supraglottic carcinoma tends to be poorly differentiated, progresses rapidly, and has a high likelihood of cervical lymphatic metastasis due to the rich lymphatic drainage in the region. Tumors originating on the laryngeal surface of the epiglottis or in the laryngeal ventricle are often hidden and difficult to detect through indirect laryngoscopy. Early lesions are more readily identified through electronic laryngoscopy. Certain tumors originating in the laryngeal ventricle may extend across anatomical boundaries, involving both the supraglottic and glottic regions, and diffusely invading the paraglottic space. These tumors, sometimes termed "transglottic cancers," tend to grow submucosally, leaving the mucosal surface relatively intact, which makes detection and pathological diagnosis challenging.
Glottic Carcinoma
Early symptoms primarily involve changes in voice, which gradually worsen, leading to hoarseness, roughness, or even aphonia. Prolonged hoarseness exceeding two weeks, unresponsive to rest and general treatment, warrants a thorough laryngeal examination.
As the narrowest part of the airway, the glottis is prone to obstruction during tumor progression. Vocal cord immobility and narrowing of the glottic space, combined with tumor-induced laryngeal cavity blockage, may cause breathing difficulties, potentially becoming life-threatening and requiring urgent intervention. Glottic carcinoma generally exhibits good differentiation and progresses slowly, with limited lymphatic drainage making early lymphatic metastases uncommon. However, invasion of the supraglottic or subglottic regions accelerates progression and increases the likelihood of lymphatic metastasis. Tumor penetration of the thyroid cartilage or cricothyroid membrane may lead to visible laryngeal swelling and anterior cervical masses.
Subglottic Carcinoma
Subglottic carcinoma refers to tumors located below the vocal cords and above the lower border of the cricoid cartilage. It is clinically rare, with early symptoms being mild and nonspecific, such as irritating cough or blood-streaked sputum. These tumors are difficult to detect through indirect laryngoscopy, increasing the risk of missed diagnoses.
Subglottic carcinoma often garners attention only after invasion of the vocal cords has caused hoarseness or airway obstruction has led to breathing difficulties. For unexplained inspiratory dyspnea or persistent irritating cough, thorough examination of the subglottic and tracheal regions is particularly important.
Examination and Diagnosis
Early diagnosis and treatment are crucial for improving survival rates in laryngeal carcinoma. Individuals over the age of 40, with a history of smoking or alcohol consumption, and who exhibit hoarseness or persistent discomfort in the throat for more than two weeks, require careful examination of the pharynx and larynx.
Palpation
Attention is paid to the morphology and mobility of the laryngeal structure, the presence of tenderness, the existence of masses in the anterior cervical soft tissue and thyroid gland, as well as enlargement of cervical lymph nodes.
Laryngoscopic Examination
Laryngoscopy serves as an important method for the morphological diagnosis of laryngeal carcinoma. The examination covers areas including the tongue base, lingual surface of the epiglottis, margins of the epiglottis, laryngeal surface of the epiglottis, bilateral aryepiglottic folds, arytenoid area, interarytenoid region, ventricular fold, laryngeal ventricle, vocal cords, bilateral pyriform sinuses, and the post-cricoid region. Observations focus on the presence of masses, ulcers, or elevations, and whether vocal cord movement is impaired.
Indirect laryngoscopy may not completely expose the laryngeal structures due to variations in epiglottic morphology or heightened gag reflexes in some patients. Fiberoptic (or electronic) nasopharyngolaryngoscopy, particularly when combined with dynamic laryngoscopy or narrow-band imaging (NBI) endoscopic technology, provides a more comprehensive view of laryngeal anatomy. It also facilitates the evaluation of vocal cord vibrations and the subglottic region, aiding in the detection of early laryngeal carcinoma and assessment of lesion boundaries.
Contrast-Enhanced CT or MRI
Contrast-enhanced CT can delineate the tumor's extent, assess involvement of the paraglottic space, pre-epiglottic space, subglottic region, and laryngeal cartilage, as well as identify invasion of extralaryngeal tissues or cervical lymph node metastasis. Contrast-enhanced MRI offers superior visualization of soft tissues but is not routinely performed before surgery. It can be selectively used for evaluating vascular and soft tissue involvement.
PET-CT
PET-CT is advantageous for identifying occult lesions, recurrence, cervical lymph node metastasis, or distant metastasis.
Biopsy
Biopsy is the gold standard for confirming a diagnosis of laryngeal carcinoma. It can be performed under indirect laryngoscopy, fiberoptic (or electronic) nasopharyngolaryngoscopy, or direct laryngoscopy. In cases where surface necrosis or submucosal tumor growth prevents obtaining tumor tissue on the first attempt, repeat biopsy may be necessary for clinically suspected malignancies with initial negative biopsy results.
Differential Diagnosis
Laryngeal Tuberculosis
Primary symptoms include throat pain and hoarseness, along with weak voice or even aphonia. Severe cases may experience intense throat pain, often interfering with eating. Laryngoscopic examination reveals pale and edematous laryngeal mucosa with superficial ulcers and mucopurulent secretions; occasionally, a tuberculoma presents as a mass-like lesion. Chest X-rays may indicate progressive pulmonary tuberculosis. Laryngeal biopsy can aid in differentiation.
Laryngeal Papilloma
The condition typically has a long disease course and may present as solitary or multiple lesions. Tumors often appear as papillomatous projections, confined to the mucosal surface without impairment of vocal cord movement. Since adult laryngeal papillomas have malignant potential, biopsy is required for differentiation.
Laryngeal Amyloidosis
Although not a true tumor, laryngeal amyloidosis arises from tissue degeneration caused by protein metabolism disorders. The main manifestation is hoarseness, and examination often reveals yellowish, firm masses located in the vocal cords, laryngeal ventricles, or subglottic region. Smooth surface texture is characteristic, and pathological examination differentiates this condition.
Laryngeal Syphilis
Patients may experience hoarseness and mild throat discomfort. Laryngoscopic examination typically shows lesions in the anterior larynx with erythematous and swollen mucosa. Raised syphilitic nodules and deep ulcers with significant tissue destruction are common. Post-healing scar contraction may cause deformity of the larynx. Serological testing and laryngeal biopsy provide a basis for differentiation.
Treatment
The primary objective of laryngeal cancer treatment is tumor control. Beyond this, efforts focus on minimizing the impact on the larynx's functions—phonation, respiration, swallowing—as well as preserving appearance, thereby improving the patient's quality of life.
The main treatment modalities for laryngeal cancer include surgery, radiotherapy, chemotherapy, targeted therapy, and immunotherapy. Early-stage laryngeal cancer can be treated with a single modality, while advanced-stage laryngeal cancer often requires a multidisciplinary approach.
Surgical Treatment
The guiding principle of surgery is the en bloc removal of the tumor with sufficient safe surgical margins. Margins have a significant impact on recurrence and prognosis. For glottic carcinoma, a margin of more than 3 mm is generally required, while margins of more than 5 mm are recommended for supraglottic and subglottic carcinomas.
Surgical methods for laryngeal cancer include minimally invasive transoral microsurgery using a suspension laryngoscope, open partial laryngectomy, and total laryngectomy. The choice of procedure involves a comprehensive evaluation of factors such as tumor location, pathology, TNM staging, patient age, and overall condition.
Transoral Surgery
Transoral CO2 laser surgery using a suspension laryngoscope is currently the most common surgical approach for early-stage laryngeal cancer. It is suitable for the treatment of early glottic and supraglottic carcinoma that is well-exposed, particularly glottic carcinoma without involvement of the anterior commissure or vocal process. Transoral plasma surgery and robot-assisted surgery have also been reported.
Advantages of transoral surgery include shorter operative time, faster postoperative recovery, no need for tracheostomy, minimal impact on phonation, respiration, and swallowing, and no impact on external appearance. Limitations include difficulties in exposure and excision due to the transoral approach, as well as challenges in judging deep margins of laryngeal cancer. Strict attention is given to surgical indications.
Partial Laryngectomy
Laryngofissure surgery is suitable for cases of glottic carcinoma (Tis, T1) where transoral surgery is not feasible and where the anterior third of the vocal cord is free from tumor involvement.
Vertical partial laryngectomy is suitable for glottic carcinomas that are primarily located in one-half of the larynx. It is also suitable for supraglottic carcinomas involving the laryngeal ventricle and vocal cord without invasion of the epiglottis, pre-epiglottic space, or paraglottic space. If the aryepiglottic fold is involved, at least partial mobility of the vocal cord is preferred, and subglottic invasion should not exceed 5 mm.
Supraglottic horizontal partial laryngectomy is suitable for supraglottic carcinomas without laryngeal ventricle involvement. It is not suitable for carcinomas involving the vocal cords, anterior commissure, arytenoid cartilage, or subglottic region. Caution is advised in cases of severe pulmonary dysfunction.
Partial laryngectomy above the cricoid cartilage is suitable for extensive glottic and supraglottic carcinomas with at least one third of the posterior vocal cord mucosa remaining normal and subglottic invasion not exceeding 5 mm.
Total Laryngectomy
Indicated for T3 and T4-stage supraglottic, glottic, or subglottic carcinoma unsuitable for partial laryngectomy; recurrent or radiotherapy-failed laryngeal cancer; and cases where pulmonary dysfunction after partial laryngectomy cannot be adequately managed. It is also considered for elderly patients in poor general condition. Total laryngectomy results in airway discontinuity, necessitating permanent tracheostomy through the anterior neck to restore the airway.
Cervical lymph node metastasis is common in laryngeal cancer. Thus, neck dissection is an integral part of laryngeal cancer surgery. Cervical lymphatic metastasis of laryngeal cancer typically follows a predictable pattern, progressing from nearby nodes to more distant ones according to the lymphatic drainage path. The choice of neck dissection technique depends on the state of lymph node metastasis and the primary tumor stage (T). Surgical approaches include radical neck dissection, extended radical neck dissection, functional neck dissection, selective neck dissection, and prophylactic neck dissection.
Radiotherapy
Radiotherapy is a key treatment modality for laryngeal cancer, with its efficacy dependent on the tumor cell's radiosensitivity and tumor extent. Radiotherapy is classified into definitive radiotherapy, preoperative or postoperative planned radiotherapy, and palliative radiotherapy.
In early-stage laryngeal cancer, the five-year survival rate with definitive radiotherapy is comparable to that of surgical treatment. However, drawbacks include a longer treatment cycle and potential complications such as loss of taste and smell, as well as dry mouth.
Drug Therapy
Chemotherapy
Chemotherapy is currently not the primary treatment option for laryngeal cancer but serves as an important component of multimodal treatment for advanced-stage disease. Chemotherapy approaches include induction, adjuvant, and palliative chemotherapy, primarily based on platinum-based regimens, either as monotherapy or in combination with other agents.
Immunotherapy
Immunotherapy is increasingly being used in clinical practice. However, its specific efficacy and side effects require further observation.
Chemoradiotherapy or Surgery Combined with Chemotherapy
These approaches are also used as treatment strategies aimed at preserving laryngeal function in laryngeal cancer.
Prognosis
Factors influencing prognosis include the primary site of the tumor, TNM staging, age, physical condition, nutritional status, treatment methods, and whether surgical margins are clean.
The 5-year survival rate for glottic carcinoma is approximately 80% to 85%, for supraglottic carcinoma it is around 65% to 75%, and for subglottic carcinoma, it is the poorest, at about 40%.
Other Types of Malignant Laryngeal Tumors
Verrucous Carcinoma
In 1948, Ackerman first classified verrucous carcinoma as a distinct subtype of squamous cell carcinoma and named it Ackerman tumor. Verrucous carcinoma is a non-metastatic, well-differentiated squamous cell carcinoma characterized by exophytic growth, a warty appearance, slow progression, and well-demarcated pushing margins. It is more common in older male patients with a history of heavy smoking and alcohol use. This carcinoma frequently occurs in regions such as the oral cavity, perineum, and cervix, while its occurrence in the larynx is rare. Verrucous carcinoma accounts for 1% to 4% of all malignant laryngeal tumors, with the anterior part of the vocal cords being the most common site, and hoarseness being the most prevalent symptom.
Clinical examination reveals a well-circumscribed, broad-based, exophytic, warty tumor with a firm texture and brownish or white coloration. Microscopically, the tumor is composed of well-differentiated keratinized squamous epithelium with a fibrovascular core and very few mitotic figures.
Verrucous carcinoma is primarily treated through surgical resection, with a generally favorable prognosis. However, local recurrence is a common feature, necessitating wide surgical margins. Neck dissection is generally not recommended unless there is clear evidence of cervical lymph node metastasis. There is no consensus on the use of radiotherapy for verrucous carcinoma. Most experts agree that its local control through radiotherapy is inferior to that of typical laryngeal squamous cell carcinoma. Consequently, radiotherapy is not usually recommended as a first-line treatment, except in cases of advanced disease or when the patient’s general condition precludes surgery. It is important to note that some verrucous carcinomas may contain squamous cell carcinoma components, referred to as hybrid tumors, which have metastatic potential.
Papillary Squamous Cell Carcinoma
Papillary squamous cell carcinoma is a distinct subtype of squamous cell carcinoma characterized by exophytic, papillary growth and a favorable prognosis. Risk factors include tobacco and alcohol abuse, although the role of HPV in its pathogenesis remains unclear.
Papillary squamous cell carcinoma of the larynx is most commonly found in the supraglottic region. Hoarseness and airway obstruction are common clinical symptoms. This carcinoma often presents as soft, fragile, exophytic, polypoid tumors. It may metastasize to cervical lymph nodes, though distant metastasis is rare. Surgery is the primary treatment choice, and its prognosis is generally better than that of typical squamous cell carcinoma.
Basaloid Squamous Cell Carcinoma
Basaloid squamous cell carcinoma is an aggressive, high-grade subtype of squamous cell carcinoma that features both basaloid and squamous cell components. It is often mistaken for adenoid cystic carcinoma. This subtype is more commonly observed in older male patients, with the pyriform sinus and supraglottic region being the most frequently affected sites.
Common symptoms include hoarseness, dysphagia, pain, and cervical masses. Laryngoscopy typically reveals a centrally ulcerated mass with extensive submucosal induration, making it easily confused with minor salivary gland tumors or other soft tissue tumors. At the time of diagnosis, approximately two-thirds of patients present with cervical lymph node metastases.
Early-stage disease may be treated with surgery alone, although recurrence is common. For advanced-stage disease, radical surgery combined with postoperative radiotherapy and chemotherapy is recommended as part of a multimodal approach. The overall prognosis for this subtype is poor.
Spindle Cell Carcinoma
Spindle cell carcinoma is a rare subtype of squamous cell carcinoma in the larynx. Microscopically, it consists of highly atypical squamous epithelium (or in situ/invasive squamous cell carcinoma) intermixed with malignant spindle cells. The spindle cells typically exhibit significant polymorphism and atypical features, are arranged in fascicles, and frequently show mitotic activity. Spindle cells often express epithelial markers.
On laryngoscopy, these lesions often appear polypoid in nature. Treatment primarily involves wide surgical resection, often supplemented with postoperative radiotherapy. The overall prognosis for spindle cell carcinoma is poor.
Adenosquamous Carcinoma
Adenosquamous carcinoma is extremely rare. The main histopathological feature is the presence of both adenocarcinoma and squamous carcinoma components. The squamous component may present as carcinoma in situ or invasive carcinoma, while the adenocarcinoma component is typically located in the deeper part of the tumor. Clinical manifestations include hoarseness, throat pain, dysphagia, and/or hemoptysis. Physical examination may reveal an exophytic or polypoid mass, or poorly defined mucosal induration with ulceration. These tumors are prone to cervical lymph node metastasis. Treatment involves wide surgical resection combined with postoperative radiotherapy and chemotherapy as part of a multidisciplinary approach. The overall prognosis is poor.
Malignant Epithelial Tumors of Non-Squamous Origin
Mucoepidermoid Carcinoma
Mucoepidermoid carcinoma is a malignant tumor arising from salivary glands, accounting for approximately 5% to 10% of salivary gland tumors. Its occurrence in the larynx is extremely rare and originates from epithelial cells of minor salivary glands. It is more commonly observed in middle-aged and elderly men and may present with symptoms such as hoarseness and respiratory distress. CT imaging may serve as a routine diagnostic tool, and pathological examination is the gold standard for diagnosis. This tumor exhibits poor sensitivity to radiotherapy, and surgical excision is currently the preferred treatment method.
Adenoid Cystic Carcinoma
Adenoid cystic carcinoma predominantly arises from salivary glands and frequently invades nerves. Its occurrence in the larynx is rare. It can affect individuals of any age, although it is more common in middle-aged adults, without significant gender differences. Due to its slow growth, early stages may be asymptomatic or manifest as painless masses, with progressive respiratory difficulties appearing later. Ancillary examinations include laryngoscopy, CT scans, and MRI, while pathological analysis is the diagnostic gold standard. Surgery, supplemented by postoperative radiotherapy, is the treatment of choice and demonstrates superior outcomes compared to surgery or radiotherapy alone.
Chondrosarcoma
Chondrosarcoma is a malignant tumor originating from the cartilaginous framework of the larynx and is the most common non-epithelial malignant tumor of the larynx, accounting for 75% of laryngeal sarcomas. It predominantly originates from ossified hyaline cartilage, with the cricoid cartilage being the most commonly affected site, followed by the thyroid cartilage. Early stages are asymptomatic and often go undetected. As the tumor enlarges, symptoms such as hoarseness and respiratory difficulties may develop. Preoperative pathological confirmation is challenging; however, CT and MRI imaging offer some diagnostic value. Compared to chondrosarcomas in other regions, laryngeal chondrosarcomas typically grow more slowly and exhibit a low rate of distant metastasis. Surgical treatment yields favorable outcomes.
Haematolymphoid Tumors
Primary non-Hodgkin lymphoma (NHL) of the hypopharynx, larynx, and trachea is extremely rare. The majority of primary laryngeal NHL cases are B-cell lymphomas, particularly diffuse large B-cell lymphoma and mucosa-associated lymphoid tissue (MALT) extranodal marginal zone B-cell lymphoma. Any part of the larynx may be affected, with the supraglottic region being the most common site. Typical symptoms include hoarseness, throat discomfort, and sore throat. The preferred treatment method is a combination of radiotherapy and chemotherapy.
Neuroendocrine Tumors
Neuroendocrine tumors are uncommon, with atypical carcinoids being the most prevalent subtype (54%), followed by neuroendocrine small cell carcinoma (34%), paraganglioma (9%), and typical carcinoid tumors. Over 90% of these tumors occur in the supraglottic region. Common symptoms include hoarseness, dysphagia, throat pain, and neck masses. Neuroendocrine tumors exhibit poor sensitivity to radiotherapy and chemotherapy. Surgery is the preferred treatment option. Due to the high rate of cervical lymph node metastasis, neck dissection is recommended even in the absence of clinically evident lymph node involvement.
Other Malignant Mesenchymal Tumors of the Larynx
Other malignant tumors of mesenchymal origin in the larynx include fibrosarcoma, malignant fibrous histiocytoma, liposarcoma, leiomyosarcoma, and rhabdomyosarcoma. Additionally, malignant melanoma of the laryngeal mucosa is an extremely rare clinical entity.