Obstructive sleep apnea (OSA) refers to episodes of apnea and hypopnea caused by upper airway collapse during sleep. It is typically associated with symptoms such as snoring, disrupted sleep architecture, frequent reductions in blood oxygen saturation, daytime sleepiness, and difficulties with concentration. OSA can lead to multi-organ and multi-system complications, including hypertension, coronary artery disease, and diabetes. OSA is categorized into adult and pediatric types, with a prevalence of approximately 2%–4% in adults and 1.2%–5.7% in children. OSA can occur at any age, but it is most common among middle-aged obese men. In severe pediatric cases, it may affect growth and development.
Key Concepts
Apnea
Apnea is defined as a total cessation of airflow at the nose and mouth during sleep (≥90% reduction from baseline), lasting at least 10 seconds in adults or at least two respiratory cycles in children. Apnea events are classified into obstructive, central, and mixed types. Obstructive apnea involves the cessation of nasal and oral airflow while thoracoabdominal respiratory effort persists. Central apnea involves cessation of breathing due to the absence of central respiratory drive, with both nasal/oral airflow and thoracoabdominal effort ceasing during the event. Mixed apnea starts as central apnea and progresses to obstructive apnea within a single episode.
Hypopnea
Hypopnea, also referred to as insufficient ventilation, is characterized by a ≥30% reduction in nasal and oral airflow intensity from baseline during sleep, accompanied by a ≥4% drop in arterial oxygen saturation (SaO2) and lasting at least 10 seconds. Alternatively, it may be defined as a ≥50% reduction in airflow, with a ≥3% drop in SaO2 or an arousal lasting at least 10 seconds. For children, hypopnea is diagnosed when airflow decreases by more than 30% from baseline, SaO2 drops by ≥3%, and the event lasts at least 10 seconds.
Arousal
Arousal refers to a shift in EEG frequency lasting more than 3 seconds during non-rapid eye movement (NREM) sleep, involving the appearance of theta waves, alpha waves, and/or EEG waves with a frequency >16 Hz (excluding spindle waves).
Respiratory Effort-Related Arousal (RERA)
RERA refers to breathing effort-related events lasting at least 10 seconds that do not meet criteria for apnea or hypopnea but are accompanied by an arousal.
Sleep Hypoxemia
Sleep hypoxemia describes a state during sleep where saturation of arterial oxygen (SaO2) drops below 90% in adults or below 92% in children due to apnea and/or hypopnea.
Apnea-Hypopnea Index (AHI)
AHI represents the total number of apneas and hypopneas per hour of sleep, calculated as AHI = (number of apneas + number of hypopneas) / total sleep time. For pediatric OSA, the obstructive apnea-hypopnea index (OAHI) is used, which is defined as the average number of obstructive apneas, mixed apneas, and obstructive hypopneas per hour of sleep.
Respiratory Disturbance Index (RDI)
RDI is the total number of events per hour of sleep, including apneas, hypopneas, and RERA events.
Etiology
The pathogenesis of OSA is complex and highly variable between individuals. It involves both anatomical and non-anatomical factors. The PALM model is commonly utilized to evaluate causes. "P" represents the critical closing pressure of the upper airway (Pcrit), reflecting the severity of anatomical factors. "A" is arousal threshold, "L" is loop gain (a measure of ventilatory control stability), and "M" is neuromuscular responsiveness; these represent non-anatomical factors. Clinical cases with a single factor responsible for OSA are uncommon.
Anatomical Factors
Nasal and Nasopharyngeal Narrowing
This includes factors causing narrowing or obstruction of the nasal cavity or nasopharynx, such as deviated nasal septum, nasal polyps, chronic rhinosinusitis, turbinate hypertrophy, adenoid hypertrophy, and nasopharyngeal stenosis or atresia. In children, adenoid hypertrophy may lead to nasal obstruction and mouth breathing, which can affect craniofacial development. Failure to address this in time may result in abnormal craniofacial development, exacerbating the condition.
Oropharyngeal Narrowing
Enlarged palatine tonsils, thickened soft palate, hypertrophy of the lateral pharyngeal walls, elongated uvula, thickened tongue base, and macroglossia can all contribute to narrowing in this region. Since the oropharyngeal cavity consists of soft tissues without cartilage or bony support, its narrowing plays a crucial role in the pathogenesis of OSA.
Narrowing of the Hypopharynx and Laryngeal Cavity
Examples include infantile epiglottis or epiglottic tissue collapse.
Developmental Abnormalities or Deformities of the Maxilla and Mandible
These are common and significant causes of OSA.
Non-Anatomical Factors
Low Arousal Threshold
Even mild airway narrowing can lead to arousal.
High Loop Gain
This is primarily caused by abnormalities in respiratory center regulation. During sleep, airway narrowing increases carbon dioxide concentration in the blood, leading to deeper and faster breathing to correct arterial partial pressure of carbon dioxide (PaCO2). After PaCO2 returns to normal, the central nervous system may fail to adjust in time, resulting in continued deep breathing, which leads to hyperventilation. A further reduction of PaCO2 below a certain threshold can then trigger apnea.
Abnormal Neuromuscular Responsiveness
This is characterized by reduced tone of genioglossus, pharyngeal wall muscles, and soft palate muscles. This is a key mechanism underlying repetitive airway collapse and obstruction in OSA patients.
Most OSA patients experience the condition due to anatomical factors combined with at least one non-anatomical factor. Chronic sleep hypoxemia may lead to abnormal regulation by the respiratory center, meaning that as the disease progresses and its duration increases, non-anatomical factors play a larger role.
Pathophysiology
OSA patients experience recurrent upper airway collapse and obstruction during sleep, leading to apnea and/or hypopnea and triggering a cascade of pathological and physiological changes.
Intermittent Hypoxia and Carbon Dioxide Retention
Apnea results in a gradual decline in arterial oxygen partial pressure and a rise in carbon dioxide partial pressure. Hypoxia can increase catecholamine secretion, which contributes to hypertension. Hypoxia may also cause arrhythmias, elevated levels of erythropoietin, increased red blood cell production, heightened platelet activity, and reduced fibrinolytic activity, potentially leading to coronary artery disease or cerebral thrombosis. Additionally, hypoxia can increase glomerular filtration, resulting in nocturia, and may disrupt the urinary reflex arc, manifesting as nocturnal enuresis in pediatric patients, with occasional enuresis seen in a small number of adult OSA patients. Hypoxia affects nearly all organ systems, and the pathological and physiological effects of OSA are similarly widespread and systemic.
Disruption of Sleep Architecture
Recurrent apnea, hypopnea, and arousal events during sleep disrupt the structure of sleep. Stage 3 sleep and REM sleep are significantly reduced, leading to lower sleep efficiency and symptoms such as daytime sleepiness, fatigue, difficulty concentrating, and memory impairment. Over the long term, these sleep disturbances may contribute to mood changes such as depression, irritability, and increased anger.
Changes in Thoracic Pressure
During sleep apnea episodes, thoracic negative pressure during inhalation increases significantly, which may result in cardiac enlargement or vascular displacement. Simultaneously, the high negative pressure in the thoracic cavity facilitates the reflux of gastric contents into the esophagus and/or pharynx, causing conditions such as reflux esophagitis or pharyngitis. Among pediatric patients, prolonged high thoracic negative pressure can contribute to thoracic deformities.
Clinical Manifestations
Symptoms
Snoring and sleep apnea often exhibit progressive worsening with age and weight gain. The snoring typically occurs intermittently, accompanied by repeated disruptions in breathing rhythm and episodes of apnea. Severe cases may present with nighttime awakenings caused by sensation of choking. These symptoms are often exacerbated in the supine position.
Excessive daytime sleepiness may range from mild to severe. Mild cases manifest as slight drowsiness and fatigue without significant impacts on daily activities or work. In severe cases, patients may experience uncontrollable sleep episodes while driving or even during conversations. Despite quick sleep onset, prolonged sleeping, and adequate sleep duration, no significant recovery in mental or physical states is observed post-sleep.
Cognitive symptoms include impaired memory, reduced attention span, and slower reaction times.
Symptoms such as dry mouth, a foreign body sensation in the throat upon waking, morning headaches, and elevated blood pressure are commonly reported.
In some severe cases, sexual dysfunction, frequent nocturia, or even enuresis may be present.
Mood and behavioral changes, such as irritability, anger, or depression, are more common in patients with a prolonged disease course and severe conditions.
In pediatric patients, additional symptoms such as craniofacial developmental abnormalities, delayed physical growth, thoracic deformities, and reduced academic performance may also occur.
Signs
General physical characteristics include obesity or noticeable overweight status in most adult patients. A short and thick neck is a common feature. Some patients may display evident developmental abnormalities of the maxilla and mandible. Other features may include a narrow external nose, upwardly tilted nostrils visible from the frontal view, and an upwardly curved upper lip. Pediatric patients often demonstrate underdeveloped physical growth compared to peers, along with craniofacial abnormalities and thoracic deformities.
Upper airway characteristics often involve narrowing of the pharyngeal cavity, particularly the oropharyngeal region. Clinical findings may include enlarged tonsils, thickened and lax soft palate, an elongated and thickened uvula, tongue base and/or tongue body hypertrophy, lymphoid hyperplasia at the tongue base, and thickened lateral pharyngeal bands. Additional findings may include adenoid hypertrophy, nasal septum deviation, turbinate hypertrophy, or nasal polyps.
Laboratory Tests
Overnight Polysomnography (PSG)
Polysomnography serves as a critical tool for evaluating sleep-related disorders. Overnight PSG is the gold standard for diagnosing OSA. Major monitoring parameters include:
Electroencephalography (EEG), electrooculography (EOG), and chin electromyography (EMG) are utilized to determine the patient’s sleep state and sleep stages. Differentiation between REM sleep and NREM sleep is achieved, allowing assessment of sleep architecture, sleep efficiency, and calculation of the apnea-hypopnea index (AHI).
Oral and nasal airflow evaluates respiratory patterns during sleep to determine the presence or absence of apnea or hypopnea.
Thoracic and abdominal respiratory effort helps discern whether respiratory movements are present during apnea episodes. Used in conjunction with oral and nasal airflow data, this parameter differentiates obstructive, central, and mixed apneas or hypopneas.
Continuous monitoring of blood oxygen levels provides an assessment of hypoxia and its fluctuations during sleep.
Body position evaluates sleep positions to understand their association with apnea or hypopnea events.
Anterior tibialis muscle EMG is primarily used in the diagnosis of restless leg syndrome, as patients with this syndrome experience repetitive and rhythmic leg movements during sleep, leading to frequent arousals and disruptions in sleep architecture, as well as excessive daytime sleepiness.
Evaluation of Sleepiness Levels
This includes both subjective and objective assessments.
Subjective assessment tools include the Epworth Sleepiness Scale (ESS), which evaluates the severity of excessive daytime sleepiness.
Objective methods include the Multiple Sleep Latency Test (MSLT), which measures the physiological tendency to fall asleep, and the Maintenance of Wakefulness Test (MWT), which assesses the ability to remain awake in a quiet and non-stimulating environment.
Diagnosis
Qualitative Diagnosis
The diagnosis of OSA is primarily based on a combination of medical history, physical signs, and PSG results. The assessment of disease severity and hypoxemia is detailed in Table 1 and Table 2.
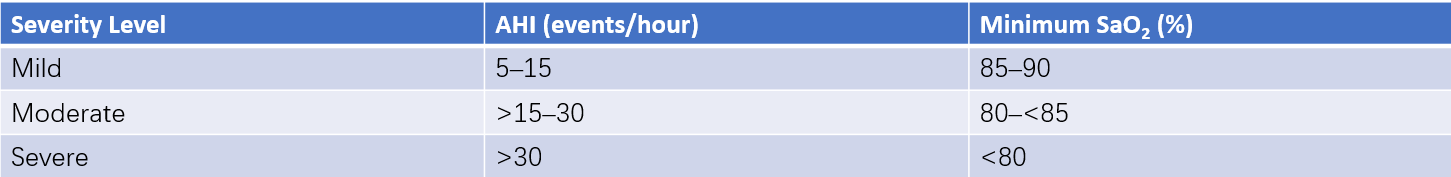
Table 1 Criteria for assessing the severity of OSA and hypoxemia in adults
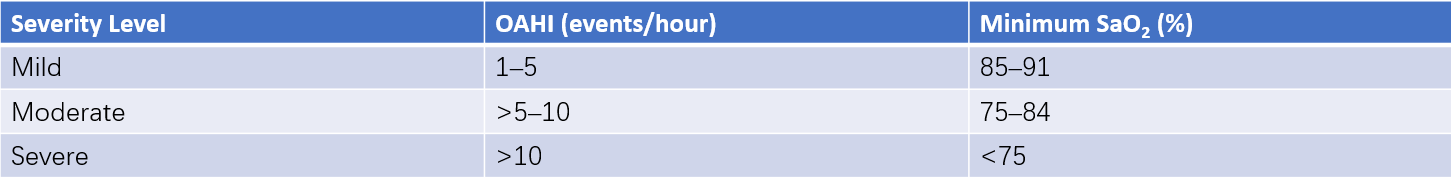
Table 2 Criteria for assessing the severity of OSA and hypoxemia in children
The severity of OSA is assessed using the apnea-hypopnea index (AHI), with documentation of the hypoxemia status. For example, an AHI of 25 events per hour and a minimum SaO2 of 88% would be reported as "moderate OSA with mild hypoxemia."
Localization of the Obstruction Plane and Related Examinations
The current main methods for evaluating the causes, conditions, and locations of upper airway obstruction in OSA patients include the following:
Electronic Nasopharyngoscopy with Müller Maneuver
This procedure involves surface anesthesia of the oropharyngeal and nasopharyngeal mucosa while the patient remains awake. An electronic nasopharyngoscope is used to examine these areas. The patient pinches their nose shut, closes their mouth, and inhales forcefully to simulate upper airway obstruction and collapse of the hypopharyngeal cavity. This allows an assessment of the degree of narrowing at the nasopharyngeal, oropharyngeal, and hypopharyngeal levels. This is one of the commonly used methods for identifying the obstruction site in the upper airway.
Esophageal Pressure (Pes) Measurement
This technique is considered the most accurate method for localization diagnosis. A catheter containing miniature pressure sensors is inserted through the nasal cavity, passing through the pharyngeal cavity and into the esophagus. The pressure sensors are positioned at various levels of the upper airway. During normal inspiration, all sensors display uniform negative pressure changes. When obstruction occurs at a certain site in the upper airway, sensors above the obstruction do not show pressure changes, enabling identification of the obstruction site.
Cranial X-Ray Cephalometry
This method is primarily utilized to evaluate the anatomical characteristics of the airway.
Upper Airway CT and MRI
CT and MRI enable two-dimensional and three-dimensional observation and measurement of the upper airway, providing more detailed information on the structural characteristics of the airway.
Drug-Induced Sleep Endoscopy (DISE)
This technique involves the use of medication to induce a sleep-like state, during which electronic nasopharyngoscopy is performed to determine the obstruction plane in OSA patients. Although the induced state differs from natural sleep, clinical practice has demonstrated that DISE is an effective method.
Differential Diagnosis
Primary Snoring
This is characterized by varying degrees of snoring during sleep at night, with an AHI of <5 events per hour and no daytime symptoms.
Upper Airway Resistance Syndrome
This condition involves varying frequencies and severities of snoring at night, increased upper airway resistance, an AHI of <5 events per hour, and symptoms such as daytime sleepiness or fatigue. Improvement with trial non-invasive ventilation supports the diagnosis.
Restless Legs Syndrome (RLS) and Periodic Limb Movement of Sleep (PLMS)
RLS is characterized by daytime drowsiness, an intense urge to move the legs at night, often accompanied by unusual discomfort, which worsens during periods of rest or while lying still and improves with activity. Symptoms often intensify before sleep. PSG monitoring shows characteristic periodic limb movements, which should be differentiated from limb movements that are associated with sleep-disordered breathing events.
Sleep Apnea Secondary to Endocrine Disorders:
Conditions such as acromegaly or hypothyroidism may present with sleep apnea.
Central Sleep Apnea-Hypoventilation Syndrome
PSG monitoring can aid in differentiation.
Treatment
Treatment approaches are individualized and multidisciplinary, depending on the underlying cause, severity of the condition, site of obstruction, and overall health of the patient.
General Treatments
Lifestyle modifications include exercise, weight loss, smoking cessation, alcohol avoidance, sleeping in a lateral position, maintaining good sleep and living habits, and avoiding excessive daytime fatigue.
Non-Surgical Treatments
Noninvasive Positive Airway Pressure Therapy
Continuous positive airway pressure (CPAP) delivered through a nasal interface is the first-line therapy for adult OSA patients. The mechanism involves using mechanical ventilation at a specific pressure to keep the upper airway open, ensuring unobstructed breathing during sleep.
Oral Appliance Therapy
This treatment is suitable for primary snoring and mild to moderate OSA, particularly in patients with mandibular retrognathia. A specialized oral device worn during sleep advances the lower jaw forward, expanding the airway behind the tongue base. Long-term use carries a risk of temporomandibular joint damage, making this therapy unsuitable for patients with severe temporomandibular arthritis or dysfunction, advanced periodontal disease, or significant tooth loss.
Pharmacological Treatment
No medication with definitive efficacy is currently available. Agents such as progesterone have been tried in clinical settings, but their effectiveness remains uncertain, and they are associated with varying degrees of adverse effects.
Surgical Treatment
Surgery is one of the important options for managing OSA. The choice of surgical procedure depends on the site and severity of the obstruction:
- For obstruction at the nasal and nasopharyngeal levels, procedures such as nasal septum deviation correction, nasal cavity expansion, or adenoidectomy may be performed.
- For oropharyngeal obstruction, procedures include uvulopalatopharyngoplasty (UPPP) and its modified techniques, soft palate shortening and anterior repositioning, soft palate pillar implants (Pillar System), tongue base suspension, hyoid suspension, upper airway radiofrequency ablation using low-temperature plasma, or hypoglossal nerve stimulation therapy (HGNS).
- For craniofacial abnormalities, maxillomandibular advancement may be undertaken.
- Tracheostomy is also a viable option for some severe OSA cases.
These surgical techniques may be performed individually or in combination, as well as in a single session or staged approach.