Nasopharyngeal angiofibroma is the most common benign tumor of the nasopharynx. It is composed of dense connective tissue, numerous elastic fibers, and blood vessels. The condition typically occurs in young males aged 10–25 years, which is why it is also referred to as "adolescent male hemorrhagic nasopharyngeal angiofibroma." The etiology remains unknown.
Pathology
The tumor originates from the periosteum of the occipital bone base, the sphenoid bone body, and the medial pterygoid process. The tumor tissue consists of a reticular stroma made up of collagen fibers and multinucleated fibroblasts, interspersed with a large number of blood vessels with thin walls and no contractility. When the tumor is damaged, it is prone to persistent bleeding. The tumor typically expands into adjacent tissues, invading the nasal cavity, paranasal sinuses, orbit, pterygopalatine fossa, and intracranial regions through foramina.
Clinical Manifestations
Bleeding
Episodic nosebleeds or oral bleeding are often the primary complaint during the patient’s first consultation. Repeated episodes of heavy bleeding can lead to varying degrees of anemia.
Nasal Obstruction
The tumor blocks the choana and extends into the nasal cavity, resulting in unilateral or bilateral nasal congestion. Associated symptoms may include nasal discharge, a nasal voice due to obstruction, reduced sense of smell, and nasal deformity.
Other Symptoms
With continued growth, the tumor can compress and resorb adjacent bones and impair the function of nearby organs. Tumor invasion of neighboring structures can cause corresponding symptoms. For example, compression of the eustachian tube orifice may lead to tinnitus or hearing loss. Orbital invasion may cause proptosis and vision impairment. Invasion of the pterygopalatine fossa could result in swelling of the cheek; nasal cavity invasion can deform the external nose. Intracranial invasion with nerve compression may lead to headaches and cranial nerve palsy.
Examinations
Anterior Rhinoscopy
Inflammatory changes are often observed in one or both nasal cavities. Retraction of the inferior turbinate may reveal a pinkish tumor in the posterior part of the nasal cavity.
Nasopharyngoscopy (Indirect, Fiberoptic/Electronic, or Endoscopic)
A rounded or lobulated reddish tumor, smooth-surfaced and rich in vascularization, is observed in the nasopharynx. Tumor invasion of the choana and nasal cavity might cause nasal deformity or soft palate depression.
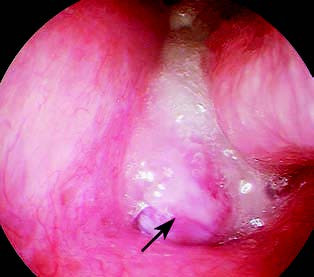
Figure 1 Nasopharyngeal endoscopy showing a fibrous vascular tumor-like lesion in the posterior nasal cavity
Palpation
Finger palpation can detect the tumor's base, which usually exhibits limited mobility and medium firmness. If the tumor has invaded the cheek region, palpation can evaluate the adhesion of the tumor pedicle to adjacent areas. Palpation, however, should be gentle because it can easily cause significant bleeding. As a precaution, palpation is rarely performed clinically.
Imaging Studies
CT and MRI scans provide clear visualization of the tumor's location, size, and shape and show the extent of its involvement with surrounding anatomic structures. Digital subtraction angiography (DSA) is helpful for assessing the tumor’s blood supply and for preoperative embolization to reduce intraoperative bleeding. The tumor is mainly supplied by the maxillary artery.
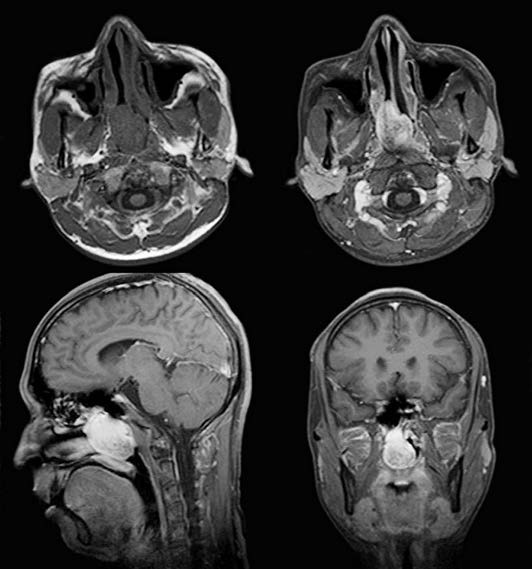
Figure 2 MRI showing a neoplasm in the right nasopharyngeal region
Diagnosis
The diagnosis is based on the patient’s history and examination results, combined with age and gender factors. Due to the tumor’s high bleeding tendency, preoperative biopsy requires caution. When the clinical history is atypical or the tumor has invaded adjacent structures, causing related symptoms, diagnosis may be challenging. Differential diagnosis may involve distinguishing the tumor from bleeding nasal polyps in the posterior choana, chordoma of the nasopharynx, and malignant tumors of the nasopharynx. Final confirmation often relies on postoperative pathological examination.
Treatment
Surgical intervention remains the primary treatment method. The surgical approach varies based on the tumor's size and location. Conventional approaches include the transpalatal approach, midfacial degloving approach, and craniofacial combined approaches. In recent years, for tumors not extensively involving the skull base or intracranial areas, endoscopic resection of nasopharyngeal angiofibroma has replaced conventional surgical techniques. Endoscopic resection allows for tumor removal while offering advantages such as minimally invasive procedures, quicker recovery, and preservation of facial aesthetics. Preoperative DSA embolization, intraoperative priority coagulation of primary blood vessels, and controlled hypotension during surgery are strategies used to minimize intraoperative bleeding.