A retropharyngeal abscess is a purulent inflammation in the retropharyngeal space, categorized into acute and chronic types based on its pathogenesis.
Etiology and Pathology
Acute Type
This is most commonly seen in children under 3 years old and is caused by purulent lymphadenitis in the retropharyngeal space. In young children, there are 3–8 lymph nodes on each side of the retropharyngeal space, and infections from the oral cavity, pharynx, nasal cavity, or sinuses can lead to inflammation of these lymph nodes, eventually resulting in abscess formation.
Other causes include foreign bodies or traumatic injuries in the pharynx that become infected, or the spread of inflammation from adjacent tissues to the retropharyngeal space. The pathogens are similar to those causing peritonsillar abscesses.
Chronic Type
This is frequently caused by cold abscess formation due to tuberculous lymphadenitis in the retropharyngeal space or cervical vertebral tuberculosis.
Clinical Manifestations
Acute cases typically have a rapid onset, with symptoms such as chills, high fever, cough, dysphagia, refusal to eat, crying and hiccupping during feeding, irritability, and a muffled voice resembling an object in the mouth. Respiratory difficulty is common, varying in severity depending on the size of the abscess, and it often worsens during sleep, sometimes accompanied by snoring. If the abscess compresses the laryngeal inlet or causes laryngeal inflammation, inspiratory difficulty becomes more pronounced.
Chronic cases usually present with systemic symptoms of tuberculosis and have a gradual onset with a prolonged course. Pharyngeal pain is typically absent, but as the abscess enlarges, patients experience a progressive sensation of pharyngeal obstruction.
Examinations
Patients with acute cases appear acutely ill, with unilateral or bilateral cervical lymphadenopathy and tenderness. Examination of the oropharynx may reveal bulging on one side of the posterior pharyngeal wall, with mucosal erythema. Larger abscesses may displace the affected palatopharyngeal arch and soft palate anteriorly. Abscesses caused by trauma or foreign bodies are often located in the hypopharynx and may only be visible with direct or indirect laryngoscopy. Abscesses resulting from cervical tuberculosis are typically midline on the posterior pharyngeal wall, with mucosa displaying a paler color.
During examinations, care must be taken to avoid rupturing the abscess. If rupture occurs, immediate positioning of the child's head downward is necessary to prevent aspiration of purulent material into the trachea, which could lead to suffocation or aspiration pneumonia.
Lateral cervical X-rays may show soft tissue swelling anterior to the cervical vertebrae. In cases caused by cervical tuberculosis, evidence of bone destruction is often observed.
Diagnosis
The diagnosis is usually straightforward based on the classic history, symptoms, and physical examination findings. Retropharyngeal abscess should be considered first in young children presenting with the aforementioned symptoms. Imaging studies, especially CT scans in addition to lateral cervical X-rays, provide significant diagnostic value by clearly delineating large blood vessels and aiding in distinguishing between abscess and cellulitis.
Complications
Asphyxia and Pulmonary Infection
Larger abscesses may compress the laryngeal cavity or cause laryngeal edema, leading to respiratory distress. Abscess rupture can result in aspiration of pus into the lower respiratory tract, causing aspiration pneumonia or, in severe cases, asphyxia and death.
Parapharyngeal Abscess
A retropharyngeal abscess may rupture into the parapharyngeal space, leading to the development of a parapharyngeal abscess.
Hemorrhage
The abscess may erode major cervical blood vessels, causing potentially fatal hemorrhage.
Treatment
Acute Type
Once diagnosed, incision and drainage of the abscess are recommended as early as possible. To prevent aspiration of pus into the trachea, the patient should be positioned supine with the head lowered. A direct or anesthetic laryngoscope is used to depress the base of the tongue, exposing the posterior oropharyngeal wall. The abscess is aspirated using a long, thick needle, followed by a vertical incision at the base of the abscess with a sharp blade. A long hemostatic clamp is used to open the incision, and all pus is aspirated. In cases where a large amount of pus flows out during the procedure and suction cannot keep up, the patient should be turned to a prone position to allow drainage of the pus. A tracheotomy may be required if necessary. Administration of sufficient broad-spectrum antibiotics is essential postoperatively to control the infection. For cases with inadequate drainage, the incision is reopened daily to allow thorough drainage until recovery.
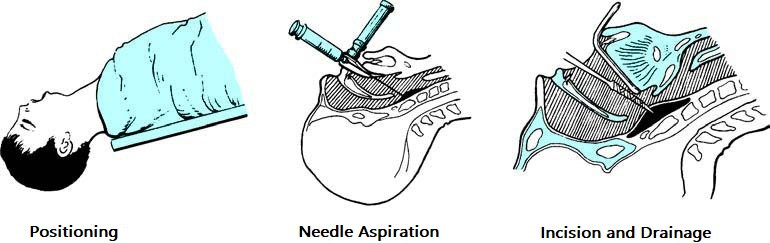
Figure 1 Surgical treatment of retropharyngeal abscess
In some primary healthcare facilities where surgical equipment is unavailable, repeated needle aspiration of the abscess may be performed, and some cases may resolve using this method.
Tuberculous Retropharyngeal Abscess
Treatment involves anti-tuberculosis therapy. Aspiration of the abscess is performed with a long, thick needle inserted orally at the abscess site. Streptomycin solution is injected into the abscess cavity, but incision and drainage via the pharynx are not recommended. For cases involving cervical vertebral tuberculosis, external drainage through a neck incision is preferred, overseen by an orthopedic specialist as part of the treatment for cervical tuberculosis.