Etiology and Pathology
Peritonsillar abscess commonly occurs as a complication of acute tonsillitis, particularly during acute exacerbations of chronic tonsillitis. Inflammatory processes within the tonsillar crypts, especially the superior tonsillar crypts, can lead to obstruction. The bacteria or inflammatory products within these crypts invade deeply, penetrate the tonsillar capsule, and spread into the peritonsillar space.
The most common pathogens include Staphylococcus aureus, Group B hemolytic streptococcus, Streptococcus viridans, and anaerobic bacteria. The condition usually presents unilaterally. Clinically, it is categorized into anterior-superior and posterior-superior types based on the location of the abscess. The anterior-superior type is more common, with the abscess located between the upper pole of the tonsil and the palatoglossal arch. The posterior-superior type, which is less common, involves the area between the tonsil and the palatopharyngeal arch.
Clinical Manifestations
The initial presentation resembles acute tonsillitis. After 3 to 4 days, persistent or worsening fever develops, accompanied by progressively severe unilateral throat pain, which intensifies during swallowing and often radiates to the ipsilateral ear or teeth. Over the next 2 to 3 days, symptoms further worsen, leading to significant pain, dysphagia, and pooling of saliva in the mouth, which may overflow. The patient may exhibit a head tilt toward the affected side, pseudorigidity of the neck, mouth slightly agape, drooling, and muffled or distorted speech. Nasal regurgitation of liquids is frequently observed. Severe cases may involve trismus, attributed to involvement of the pterygoid muscles. Ipsilateral submandibular lymphadenopathy is often present. Generalized symptoms include fatigue, reduced appetite, myalgia, and constipation.
Examinations
Patients typically show signs of acute distress. In early stages, significant erythema of the palatoglossal arch on one side may be evident. Marked swelling and restricted mouth opening suggest abscess formation. In anterior-superior cases, the affected palatoglossal arch and soft palate appear swollen and erythematous, with uvular edema and deviation toward the unaffected side. Swelling above the palatoglossal arch may obscure the tonsil and displace it inferiorly. In posterior-superior cases, the palatopharyngeal arch appears erythematous and bulging in a cylindrical manner, and the tonsil is displaced anteroinferiorly.
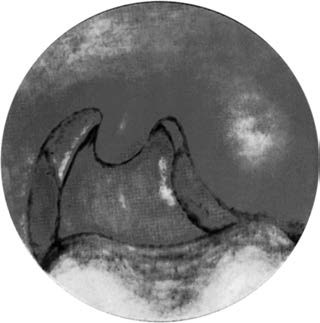
Figure 1 Peritonsillar abscess (left side)
Diagnosis
The diagnosis is usually straightforward based on clinical history and physical examination. Ultrasound evaluation can assist in differentiating peritonsillitis from a peritonsillar abscess. Aspiration of purulent material from the site confirms the diagnosis.
Differential Diagnosis
Parapharyngeal Abscess
This involves purulent inflammation in the parapharyngeal space, with abscess formation between the lateral pharynx and the ipsilateral cervical mandibular angle. Tenderness is often present. The ipsilateral tonsil and lateral pharyngeal wall are displaced toward the contralateral side, but the tonsil itself remains unaffected.
Pericoronitis of the Third Molar
This frequently occurs around impacted lower third molars. Examination reveals swollen tissue covering the crown of the tooth, often with ulceration and suppuration. Inflammation may extend to the palatoglossal arch, but the tonsils and uvula are typically unaffected.
Complications
Infection can spread to the parapharyngeal space, resulting in parapharyngeal abscess. Descending extension may lead to cervical abscess or complications such as laryngitis and laryngeal edema, with corresponding symptoms.
Treatment
Before Abscess Formation
Treatment follows the approach for acute tonsillitis, using adequate doses of antibiotics and corticosteroids to control inflammation.
After Abscess Formation
Needle Aspiration of the Abscess
Surface anesthetization with 1%–2% dyclonine is conducted before inserting the needle into the most prominent area of the abscess. Attention must be paid to the direction and depth of puncture to avoid injury to major vessels in the parapharyngeal space. Purulent material is aspirated from the abscess cavity to confirm diagnosis and provide relief.
Incision and Drainage
For anterior-superior abscesses, an incision is made at the site of needle aspiration, or at the most prominent and softened area. Alternatively, the incision may be located slightly lateral to the intersection of an imaginary horizontal line along the root of the uvula and a vertical line extending from the lower edge of the palatoglossal arch at its junction with the tongue base. The incision extends through the mucosa and superficial layers, and a long curved clamp is inserted along the muscle fibers to open the abscess cavity and drain it thoroughly.
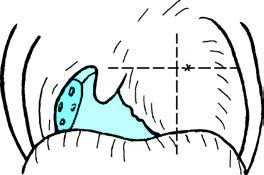
Figure 2 Incision site for peritonsillar abscess drainage
Midpoint of the line connecting the root of the uvula and the last molar
For posterior-superior abscesses, the incision is made along the palatopharyngeal arch to facilitate drainage. Follow-up evaluations are conducted the next day, and further drainage may be performed if necessary.
Tonsillectomy
After confirmation of a peritonsillar abscess and effective control of the infection with antibiotics, tonsillectomy of the affected side may be performed. This procedure ensures complete drainage, faster recovery, and prevents recurrence. For cases of recurrent abscesses, tonsillectomy is recommended 2 weeks after resolution of inflammation.