Indications
As an immune organ, the tonsils have physiological functions, particularly in children, where they play an important role in protecting the body. Arbitrary removal of the tonsils can lead to the loss of local immune response and even impair immune surveillance. Therefore, indications for tonsillectomy must be strictly observed.
- Recurrent acute episodes of chronic tonsillitis, or repeated complications such as peritonsillar abscess.
- Excessive tonsillar hypertrophy causing obstruction to swallowing, breathing, or phonation.
- Chronic tonsillitis that has become a "focus infection" causing lesions in other organs or is associated with diseases in adjacent organs.
- Tonsillar keratosis or diphtheria carriers unresponsive to conservative treatment.
- Various benign tonsillar tumors, which can be removed along with the tonsil. For malignant tumors, indications for surgery and the extent of resection should be carefully considered.
Contraindications
Surgery is generally not performed during acute inflammation; tonsillectomy is typically done 2–3 weeks after the inflammation subsides.
Patients with hematologic disorders or coagulation abnormalities, such as aplastic anemia, idiopathic thrombocytopenic purpura, or allergic purpura, are typically not candidates for surgery. If tonsillar inflammation exacerbates a hematologic condition, surgery should proceed only with thorough preparation, meticulous technique, and comprehensive perioperative management.
Severe systemic diseases, including active pulmonary tuberculosis, rheumatic heart disease, congenital heart disease, arthritis, nephritis, hypertension, and mental illnesses, are contraindicated.
During outbreaks of respiratory tract infections such as poliomyelitis or influenza, as well as during other acute infectious disease epidemics, or while the patient has an ongoing upper respiratory tract infection, surgery is not recommended.
Women during menstruation, premenstrual periods, pregnancy, or postpartum are not suitable candidates for surgery.
Patients with family histories of immunoglobulin deficiency or autoimmune diseases, or who have particularly low white blood cell counts, are not suitable for surgery.
Surgical Methods
Tonsillectomy can be performed using the dissection method, the guillotine method, or the low-temperature plasma method.
Tonsillar Dissection
This is a commonly used method. Historically, it was often done under local anesthesia, but for uncooperative children, general anesthesia is utilized. After anesthesia, the tonsil is grasped with tonsillar forceps, and an incision is made along the edge of the palatoglossal and palatopharyngeal arches using a curved knife. The tonsil capsule is then separated with a dissector, followed by its dissection from top to bottom. The lower pole of the tonsil is removed completely using a tonsillar snare. Hemostasis is achieved at the surgical site.
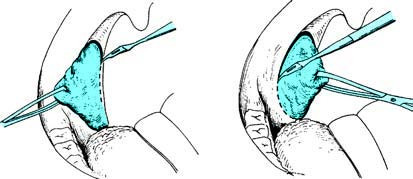
Figure 1 Incision of the mucosa
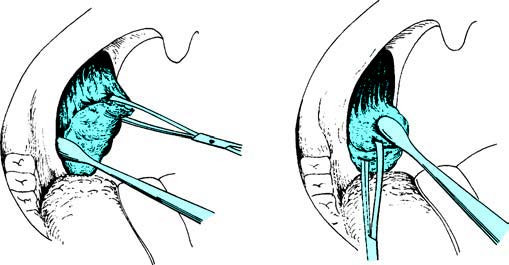
Figure 2 Separation of the tonsil
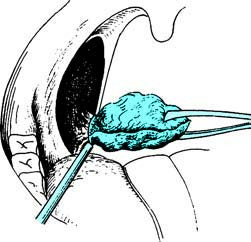
Figure 3 Removal of the tonsil
Guillotine Tonsillectomy
This method was more commonly used for children with tonsillar hypertrophy and performed historically under local or no anesthesia. However, due to the potential for psychological trauma and the risk of soft palate tearing in children under such conditions, this method is now rarely used. Currently, low-temperature plasma tonsillectomy under general anesthesia is largely preferred.
Low-Temperature Plasma Tonsillectomy
This method is generally performed under general anesthesia and includes both extracapsular and intracapsular resections. The tonsils are first grasped with tonsillar forceps to expose the upper pole. Using a plasma blade, the tonsil is excised completely from top to bottom, either along the external capsule space (extracapsular resection) or within the tonsillar capsule (intracapsular resection). The plasma blade simultaneously cuts, coagulates, irrigates, and aspirates, providing clear visualization of the surgical field and minimizing collateral damage during the procedure.
Postoperative Management
Postoperative Positioning
For patients under general anesthesia, a semi-prone position without a pillow should be used until consciousness is regained. Patients under local anesthesia should lie flat if they are children, while adults may adopt either a flat or semi-sitting position.
Diet
A cold liquid diet is recommended 4–6 hours postoperatively, transitioning to a semi-liquid diet the following day.
Monitoring for Bleeding
Patients should continuously spit out any saliva collected in the mouth instead of swallowing it. Slight blood streaks in saliva are generally not a concern, but persistent spitting of fresh blood or frequent swallowing movements in children under general anesthesia necessitate immediate examination and timely hemostasis.
Formation of a White Membrane at the Wound Site
By the second postoperative day, a layer of white membrane typically forms in the tonsillar fossa. This is a normal response, serving as a protective layer for the wound. In the absence of infection, the white membrane generally sloughs off completely within 3–4 weeks.
Wound Pain
Pain at the surgical site is more pronounced within the first 24 hours postoperatively. Analgesic or sedative medications can be administered as appropriate.
Surgical Complications and Their Management
Bleeding
Primary bleeding occurs within the first 24 hours postoperatively. The most common causes include inadequate intraoperative hemostasis, residual tissue, or rebound effects from adrenaline. Excessive postoperative pharyngeal activity, such as coughing or swallowing, can also contribute.
Secondary bleeding often occurs 5–6 days postoperatively, coinciding with the onset of white membrane sloughing. Careless eating that scratches the wound site or concurrent infections may lead to secondary bleeding. The following approaches are used for management of bleeding:
If blood clots are present in the tonsillar fossa, they should be removed, and gauze pressure should be applied for at least 10–15 minutes. Alternatively, hemostatic powder or absorbable gelatin sponge may be applied to the bleeding site, followed by compression with gauze balls. In pediatric patients, if bleeding cannot be controlled through compression, hemostasis under general anesthesia may be considered.
For active bleeding sites, bipolar electrocoagulation may be used for hemostasis, or the bleeding point may be clamped with hemostatic forceps followed by ligation or suturing.
For diffuse oozing of blood that cannot be controlled through gauze compression, sterilized gauze may be packed into the tonsillar fossa, and 3–4 stitches can be placed to suture together the palatoglossal and palatopharyngeal arches. The gauze may be left in place for 1–2 days.
In cases of excessive blood loss, treatments such as fluid replacement and blood transfusion should be initiated promptly.
Wound Infection
Postoperative wound infection may present as a sudden spike in body temperature within 3 days after surgery, or a persistent fever higher than 38.5°C. Accompanying signs include swelling of the palatal arches, uneven or absent white membrane formation on the wound site, increased pharyngeal pain, and enlargement with tenderness of the submandibular lymph nodes. Antibiotic therapy should be initiated promptly.
Pulmonary Complications
If excessive blood or foreign material enters the lower respiratory tract during the surgery and imaging confirms lung involvement, bronchoscopy should be performed to remove the blood or debris. Adequate doses of antibiotics should also be administered. With low-temperature plasma tonsillectomy, such complications are rare due to minimal intraoperative bleeding.