Etiology
The exact causes remain unclear, but related factors reported in the literature include the following:
Prolonged chronic inflammation may lead to extensive squamous metaplasia of the sinus mucosal epithelium, forming a basis for the development of squamous cell carcinoma.
Frequent exposure to carcinogenic substances, such as prolonged inhalation of certain irritants or chemical compounds including nickel, arsenic, chromium and its compounds, as well as hardwood and softwood dust, increases the risk of malignant tumors in the nasal cavity and paranasal sinuses.
Malignant transformation of benign tumors, such as recurrent nasal polyps or inverted papillomas with multiple surgeries, carries a risk of malignancy. Additionally, conditions such as rhinoscleroma, pleomorphic adenomas of minor salivary glands, schwannomas, and fibromas may also undergo malignant transformation.
Radiation exposure, whether due to radiation therapy for neighboring malignancies (e.g., nasopharyngeal carcinoma) or for benign conditions of the nasal cavity and sinuses, may result in the development of malignant tumors several years later. This highlights the risk associated with the misuse of radiotherapy.
Trauma is often recalled in the medical history of patients with sarcomas.
Pathology
Malignant tumors of the nasal cavity and sinuses include various types originating from epithelial and mesenchymal tissues. Epithelial-origin malignancies include squamous cell carcinoma, lymphoepithelial carcinoma, undifferentiated carcinoma, transitional cell carcinoma, carcinoma arising from papilloma, and basal cell carcinoma. Mesenchymal-origin malignancies include melanoma, malignant lymphoma, and sarcomas. Sarcomas account for 10%-20% of all malignant tumors in the nasal cavity and sinuses and are most commonly found in the nasal cavity and maxillary sinus. Soft tissue sarcomas include fibrosarcoma, reticulum cell sarcoma, chondrosarcoma, and rhabdomyosarcoma.
Clinical Manifestations
The clinical manifestations vary depending on the tumor's primary site and extent of involvement.
Malignant Tumors of the Nasal Cavity
Most cases result from the direct spread of malignant tumors from the sinuses, external nose, orbit, or nasopharynx. Primary malignant tumors originating in the nasal cavity are rare but can arise from any location within the cavity, most commonly on the lateral wall, such as the middle turbinate, middle meatus, or inferior turbinate, with a smaller proportion originating from the nasal septum. Symptoms often include unilateral blood-streaked nasal discharge and nasal obstruction, which are nonspecific nasal symptoms.
Malignant Tumors of the Maxillary Sinus
The primary site of maxillary sinus malignancies significantly affects their clinical presentation, treatment outcomes, and prognosis. Ohngren proposed an imaginary plane extending from the mandibular angle to the ipsilateral medial canthus, referred to as the "malignant plane," dividing the maxillary sinus cavity into an anteroinferior and a posterosuperior portion. Additionally, an imaginary vertical plane through the center of the ipsilateral pupil divides the cavity into anteroinferomedial, anteroinferolateral, posterosuperolateral, and posterosuperomedial sections.
Tumors arising in the anteroinferomedial section often present with early dental symptoms, facilitating early diagnosis and complete resection, which results in a better prognosis. Tumors from the posterosuperolateral section more easily invade the orbit, zygomatic region, or infratemporal fossa, leading to a poor prognosis. Tumors arising from the posterosuperomedial section exhibit late-onset symptoms, often invade adjacent orbital or cranial structures early on, and are difficult to completely excise, resulting in a worse prognosis.
Sbileau suggested dividing the maxillary sinus cavity into upper and lower sections along an imaginary horizontal plane through the inferior margin of the middle turbinate. Tumors in the upper section more readily invade the skull base via the ethmoid sinus or orbit, leading to a poor prognosis. Early-stage tumors are often small and localized to a specific portion of the sinus cavity, frequently in the upper medial region, and may lack obvious symptoms. As the tumor progresses, the following symptoms may develop sequentially:
Unilateral Purulent and Bloody Nasal Discharge
Persistent unilateral purulent and bloody nasal discharge warrants attention, with a foul odor occurring in advanced stages.
Pain or Numbness in the Cheek Region
Tumor invasion of the infraorbital nerve causes ipsilateral cheek pain or numbness, which can be the initial symptom and plays an important role in early diagnosis.
Unilateral Progressive Nasal Obstruction
Tumor growth leading to inward displacement or destruction of the lateral nasal wall and invasion into the nasal cavity causes this symptom.
Unilateral Molar Pain or Loosening
Tumor invasion into the alveolar ridge is responsible for this symptom. Patients often initially seek treatment from the dentistry department with misdiagnosis as a dental issue, but symptoms persist after tooth extraction.
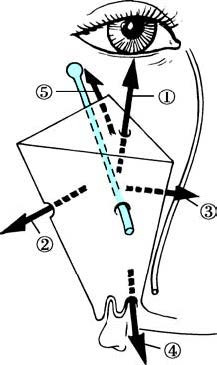
Figure 1 Illustration of the invasion of malignant tumor in the right maxillary sinus to surrounding areas
1, Destructing the orbit floor, causing eyeball displacement and resulting in diplopia;
2, Expanding toward the face, causing cheek swelling;
3, Invading the nasal cavity through the medial wall;
4, Destroying the alveolar process or hard palate and entering the oral cavity;
5, Invading the pterygopalatine fossa posteriorly.
In advanced stages, malignant tumors of the maxillary sinus may destroy the sinus walls and extend into adjacent structures, causing additional symptoms:
Cheek Swelling
Tumor compression and destruction of the anterior wall cause cheek swelling, facial asymmetry, and deformity. Perforation of the periosteum, along with invasion into cheek soft tissues or skin, may lead to fistula formation or ulceration.
Ocular Symptoms
Tumor compression of the nasolacrimal duct may cause excessive tearing. Upward pressure on the orbital floor may lead to upward displacement of the eyeball. Palpation may reveal elevation of the orbital floor and thickening or loss of definition in the orbital rim.
Hard Palate Bulging
Tumor invasion into the lower part of the sinus may cause semicircular bulging of the hard palate or the labiogingival sulcus, which may progress to ulceration, thickening of the alveolar ridge, or loosening and loss of teeth.
Difficulty in Opening the Mouth
Tumor invasion into the pterygopalatine fossa and the medial pterygoid muscle may cause persistent neuralgia and limited mouth opening. This symptom is more common in advanced stages and is associated with a poor prognosis.
Involvement of the Skull Base
Tumor extension through the nasal roof and cribriform plate into the base of the anterior cranial fossa, or lateral wall destruction spreading into the infratemporal fossa, may reach the base of the middle cranial fossa. Symptoms such as limited mouth opening, temporal swelling, headache, and earache may occur.
Cervical Lymph Node Metastasis
Cervical lymph node metastasis, most commonly involving the ipsilateral submandibular lymph nodes, may occur in advanced stages.
Malignant Tumors of the Ethmoid Sinus
In the early stages, tumors confined to the ethmoid cells may be asymptomatic. When the tumor invades the nasal cavity, symptoms such as unilateral nasal obstruction, blood-stained nasal discharge, headache, and olfactory disturbances may manifest. In advanced stages, the tumor can expand in multiple directions, causing clinical manifestations related to the involvement of adjacent structures and organs. The tumor often invades laterally through the lamina papyracea into the orbit, displacing the eyeball outward, forward, downward, or upward, potentially accompanied by diplopia. Tumors in the posterior ethmoid sinus may invade the retrobulbar area and orbital apex, leading to orbital apex syndrome. Anterior tumor progression may cause a swelling near the inner canthus. Superior invasion into the roof of the ethmoid may involve the dura mater or intracranial structures, resulting in severe headaches. Ipsilateral submandibular or deep cervical lymph node metastasis is common.
Malignant Tumors of the Frontal Sinus
Primary malignant tumors of the frontal sinus are very rare and are often asymptomatic in the early stages. As the tumor progresses, symptoms such as frontal fullness, skin numbness, and nasal bleeding may appear. Tumor invasion towards the inferolateral region may cause swelling in the frontal area and the supraorbital medial margin, with displacement of the eyeball downward, outward, or forward, along with restricted movement upward or inward. This can cause proptosis and diplopia. In advanced stages, tumor invasion into the anterior cranial fossa may cause severe headaches and signs of meningeal irritation. Lymph node metastasis frequently involves the ipsilateral submandibular or deep cervical lymph nodes.
Malignant Tumors of the Sphenoid Sinus
Primary malignant tumors of the sphenoid sinus are rare, although tumors originating in the nasal cavity, nasopharynx, posteromedial ethmoid sinus, or pituitary gland may extend into the sphenoid sinus. Occasionally, metastases from distant organs may involve the sphenoid sinus. Early stages are usually asymptomatic. As the tumor progresses, symptoms such as persistent headaches in the cranial vertex, deep orbital region, or occipital area, often radiating to the posterior neck, may occur. Imaging techniques such as X-ray tomography, CT, and MRI scans are helpful in determining the tumor's origin and extent. Metastasis is rarely observed clinically, as patients often succumb to extensive skull base or intracranial invasion before significant metastasis occurs.
Diagnosis
Due to the anatomical complexity and concealed location of the paranasal sinuses, malignant tumors often present without obvious early symptoms. High suspicion for paranasal sinus malignancy is warranted in cases of unilateral progressive nasal obstruction, blood-stained nasal discharge, unilateral facial pain or numbness, and unilateral maxillary molar pain or loosening, particularly in patients over 40 years old.
Anterior and Posterior Rhinoscopy
Examination may reveal a cauliflower-like neoplasm in the nasal cavity with a broad base, often accompanied by surface ulceration or necrosis and a tendency to bleed on touch. In the absence of a visible tumor, signs such as medial displacement of the lateral nasal wall, bloodstains, polyps, or neoplasms in the middle meatus or olfactory cleft should be carefully assessed. Posterior rhinoscopy should focus on the posterior nasal cavity, nasopharyngeal roof, Eustachian tube orifices, and the pharyngeal recess.
Nasal Endoscopy
Nasal endoscopy allows for a clearer observation of the tumor's primary location, size, shape, and involvement of the middle meatus, olfactory cleft, sphenoethmoidal recess, and sinus openings. In suspected cases of maxillary sinus malignancy, tissue can be accessed for direct examination of internal lesions by puncturing the canine fossa or inferior meatus with a cannula needle and inserting the endoscope. In many cases, nasal endoscopy of the maxillary sinus is performed concurrently with diagnostic surgery. If frozen-section histopathological analysis confirms malignancy, further surgical strategies or treatment plans are determined based on the histopathological classification.
Pathological Examination and Cytology
Pathological analysis of tumor tissue and cytology from sinus aspirates provide definitive diagnostic confirmation. Any unilateral nasal or sinus neoplasm should be submitted for pathological or cytological examination. Repeated specimen collection and analysis may be required when necessary. For tumors extending into the nasal cavity, samples can be obtained transnasally. Sinus tumors can be evaluated using aspirated cytological smears. Maxillary sinus tumors can be sampled through cannula puncture for histopathological evaluation under nasal endoscopy.
Imaging Studies
CT or MRI scans of the paranasal sinuses, with or without contrast enhancement, are the preferred imaging methods to determine tumor size and extent of invasion. PET-CT can identify differences in biochemical metabolism between various tissues by analyzing parameters such as local blood flow, oxygen utilization, and glucose metabolism. This provides valuable information for early diagnosis, tumor localization, metastasis detection, and evaluation of residual or recurrent disease.
Surgical Exploration
In cases where there is strong clinical suspicion of paranasal sinus malignancy but pathology results are inconclusive after repeated examinations (e.g., in sphenoid sinus lesions), surgical exploration of the sinuses may be considered. Intraoperative frozen-section pathology can facilitate a confirmed diagnosis.
Treatment
Due to the diverse pathological types, the difficulty of early detection, and the complex surrounding anatomical structures involving the skull, orbit, and facial aesthetics, treatment plans are typically developed through a multidisciplinary consultation approach. This often includes experts in chemotherapy, radiotherapy, imaging, and pathology.
Treatment strategies are determined based on the pathological type of the tumor, the primary site, the extent of invasion, and the patient's overall condition. A comprehensive treatment approach involving surgery, radiotherapy, chemotherapy, and biological therapies is recommended. The initial treatment is critical to the success of therapy.
Radiotherapy
Radiotherapy is a major component of comprehensive treatment. Depending on the condition, it may be administered either preoperatively or postoperatively, with intensity-modulated radiotherapy being recommended. Radical radiotherapy alone is considered for radio-sensitive malignant tumors, such as sarcomas and undifferentiated carcinomas, although the efficacy is often limited.
Palliative radiotherapy alone may be applied for advanced cases unsuitable for radical surgical resection. It may also be used for recurrent cases after surgery and in patients unable to tolerate surgery, though the outcomes are generally suboptimal.
Surgical Treatment
Surgery is the primary treatment for the majority of malignant sinonasal tumors, particularly for early-stage tumors with relatively localized involvement. In cases with extensive tumors or complex surrounding structures where complete resection is challenging, preoperative or postoperative radiotherapy or chemotherapy should be used to reduce recurrence rates and improve efficacy.
Malignant Tumors of the Maxillary Sinus
Treatment options may include endoscopic surgery, Denker's surgery, lateral rhinotomy, partial maxillectomy, or total maxillectomy, with orbital exenteration if necessary. Tumors confined to the maxillary sinus without adjacent invasion can be removed endoscopically. For hard palate defects after total maxillectomy, reconstruction may involve preserved mucoperiosteum or postoperative installation of a prosthetic obturator.
Malignant Tumors of the Ethmoid Sinus
Treatment may include endoscopic tumor resection, external ethmoidectomy, or lateral rhinotomy. For cases with significant intracranial involvement, a combination of endoscopic cranial surgery or craniofacial surgical approaches may be employed.
Malignant Tumors of the Frontal Sinus
Treatment options include endoscopic surgery or external frontal sinus surgery, where the tumor, along with the sinus mucosa, is completely removed. Bone flaps from the frontal bone should be repositioned as much as possible to preserve facial appearance. If needed, resection of all sinus walls may be performed, followed by immediate or staged frontal reconstruction surgery.
Malignant Tumors of the Sphenoid Sinus
Complete surgical resection with safe margins is challenging. Endoscopic surgery is used to remove as much of the tumor as possible, combined with preoperative or postoperative chemotherapy and radiotherapy.
Chemotherapy
Chemotherapy regimens should be selected based on the biological characteristics of the tumor and its sensitivity to chemotherapeutic agents. Options include preoperative induction chemotherapy, concurrent chemoradiotherapy, or postoperative concurrent chemoradiotherapy. Additionally, with advancements in interventional radiology, super-selective vascular intervention has allowed for the delivery of anti-tumor drugs directly into the tumor’s blood supply to target and kill cancer cells.
Prognosis
Due to the non-specific early symptoms of sinonasal malignancies, early detection and diagnosis are often difficult. Delayed treatment leads to poor prognosis in the majority of cases. Even with comprehensive treatment approaches, the 5-year survival rate for maxillary sinus carcinoma is only 30–40%. Early diagnosis and timely intervention are therefore crucial for improving survival outcomes.