The anatomical proximity of the nasal cavity and paranasal sinuses to the cranial base provides the basis for rhinogenic intracranial complications:
- Bony structures: The roof of the nasal cavity (cribriform plate), the roof of the ethmoid sinus, and the posterior wall of the frontal sinus constitute the bony base of the anterior cranial fossa. If these structures are congenitally defective, the mucosa of the nasal cavity and sinuses is in direct contact with the dura mater.
- Vascular connections: The venous drainage of the frontal sinus mucosa is connected to the veins of the dura mater and arachnoid. The diploic veins of the frontal bone drain into the superior sagittal sinus, while the diploic veins of the sphenoid bone drain into the cavernous sinus.
- Neural pathways: The sheath of the olfactory nerve is a continuation of the dura mater, with a potential communication between the subdural space of the sheath and the subdural space of the cranial cavity.
Consequently, when immunity is compromised, infections, trauma, surgical injury, or secondary infections related to foreign bodies in the nasal cavity or sinuses may spread intracranially through these routes. Frontal sinusitis and ethmoid sinusitis are the most common causes, followed by sphenoid sinusitis, while maxillary sinusitis is rare. Based on the pathways of rhinogenic infection and the severity of the disease, rhinogenic intracranial complications can be categorized into five types:
- Epidural abscess
- Subdural abscess
- Purulent meningitis
- Brain abscess
- Cavernous sinus thrombophlebitis
-
It is important to note that multiple intracranial complications (2–3 types) may occur simultaneously. These can also be accompanied by orbital complications, such as acute frontal sinusitis causing osteomyelitis, subperiosteal abscess, extradural abscess, brain abscess, and orbital subperiosteal abscess, along with orbital infections.
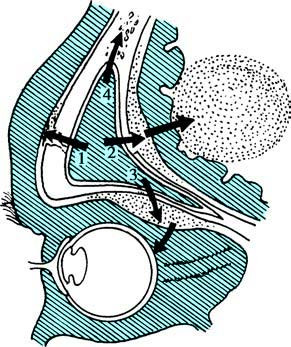
Figure 1 Complications of frontal sinusitis
1, Subperiosteal abscess caused by spread through the anterior wall.
2, Epidural abscess and brain abscess caused by spread through the posterior wall.
3, Subperiosteal abscess of the orbital wall and other orbital infections caused by spread through the inferior wall.
4, Osteomyelitis formed within the frontal bone.
Clinical Manifestations
Epidural Abscess
This condition often results from acute frontal sinusitis and frontal bone osteomyelitis. Besides symptoms of the primary disease, patients may experience progressively worsening headache, exacerbated in the supine position, and symptoms of increased intracranial pressure, such as vomiting and bradycardia. Cerebrospinal fluid (CSF) examination typically reveals no abnormalities or shows only reactive protein elevation.
Subdural Abscess
This involves diffuse or encapsulated pus accumulation in the subdural space. Advanced stages often result in purulent meningitis or other intracranial infections. Symptoms may include headache, fever, elevated intracranial pressure, and elevated CSF cell count and protein levels. Due to the non-specific nature of symptoms, imaging techniques such as CT or MRI are essential for diagnosis.
Purulent Meningitis
In cases caused by sinusitis, the onset is generally slow, while those caused by nasal-cranial trauma or surgical damage to the cranial base have a more acute onset. Symptoms and signs are similar to meningitis of other origins, including severe headache, fever, seizures, lethargy, agitation, or coma. Lumbar puncture can aid in confirming the diagnosis.
Brain Abscess
Frontal lobe abscesses caused by frontal sinusitis are more common, while temporal lobe abscesses caused by sphenoid sinusitis are less frequent. Symptoms typically include severe headache, vomiting, papilledema, and optic nerve atrophy. Abscesses in different intracranial regions can result in corresponding clinical symptoms. CT imaging is particularly valuable for diagnosis.
Cavernous Sinus Thrombophlebitis
This condition can be caused by sphenoid sinusitis or rhinogenic orbital complications. Initial symptoms include signs of septicemia, followed by obstruction of the ophthalmic venous return and paralysis of cranial nerves II–VI. Since the cavernous sinuses communicate bilaterally, advanced stages may involve the contralateral side. If accompanied by purulent meningitis, the mortality rate can be high. Early symptoms include fever, headache, photophobia, diplopia, and periorbital edema. Later stages may involve classic symptoms such as ptosis, proptosis, paralysis, chemosis, and vision loss, potentially leading to meningitis or brain abscesses.
Diagnosis
Patients with rhinogenic intracranial complications often present with clinical manifestations of sinusitis infections alongside the symptoms and signs described above. These cases require careful consideration of potential intracranial complications and prompt imaging investigations. Lumbar puncture is recommended when necessary to confirm the diagnosis.
Treatment
The treatment strategy involves using antibiotics that penetrate the blood-brain barrier to control infection. In cases of abscess formation, the affected sinuses should be surgically opened as early as possible. For extradural abscesses, necrotic sinus walls should be removed during surgery until healthy tissue is reached, with the dura mater adequately exposed to allow complete abscess drainage. Collaboration with neurosurgeons is advised for further management.