The anatomical proximity of the paranasal sinuses to the orbit allows sinus infections to cause orbital complications, which are more commonly observed in children.
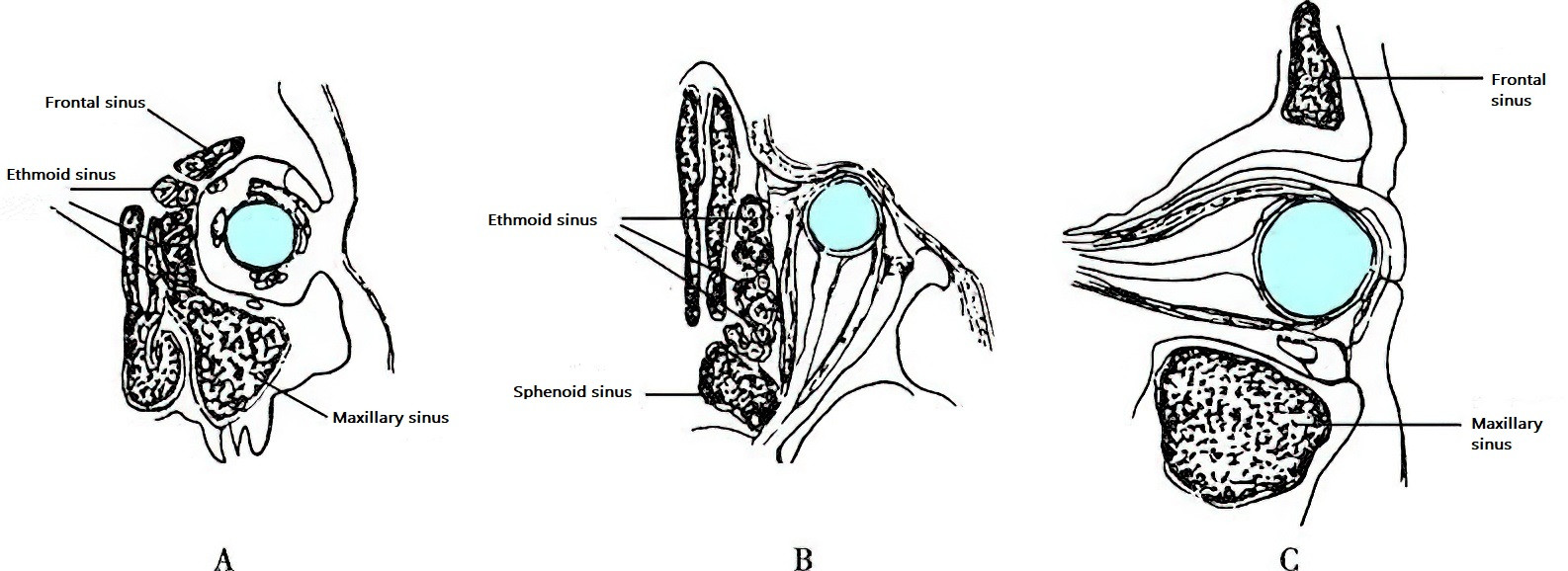
Figure 1 The relationship between the paranasal sinuses and the orbit
A. Coronal section through the orbit showing the relationship between the frontal sinus, ethmoid sinus, and the orbit.
B. Horizontal section through the orbit showing the relationship between the ethmoid sinus, sphenoid sinus, the medial orbital wall, and the orbital apex.
C. Sagittal section through the orbit showing the relationship between the frontal sinus, maxillary sinus, and the orbit.
The mechanisms by which sinus infections lead to orbital complications include:
- Direct extension of bacteria from the infected sinuses to the orbit via anatomical pathways.
- Communication between the venous networks of the sinuses and the orbit.
- Secondary infections following trauma or surgical damage to the sinus walls adjacent to the orbit.
- Weakened immune defenses in the host.
Based on disease progression, orbital complications of sinus infections can be classified into five types:
- Periorbital Cellulitis
- Subperiosteal Orbital Abscess
- Orbital Cellulitis
- Orbital Abscess
- Retrobulbar Neuritis
These orbital complications can further spread through the orbital venous system, superior orbital fissure, or other structures, leading to intracranial complications.
Clinical Manifestations
Periorbital Cellulitis (Preseptal Cellulitis)
Also referred to as inflammatory orbital edema, preseptal cellulitis is the most common and earliest rhinogenic orbital complication. Initial symptoms include eyelid hyperemia, edema, and mild tenderness. Swelling caused by ethmoid sinusitis, maxillary sinusitis, or frontal sinusitis begins in the medial canthus, lower eyelid, or upper eyelid, respectively. There is no restriction of eye movement, proptosis, displacement, or vision loss.
Subperiosteal Orbital Abscess
This complication frequently occurs in the orbital walls adjacent to the sinuses. Thrombophlebitis in the bony wall may lead to periostitis, necrosis, and the formation of a subperiosteal abscess between the orbital periosteum and the bone.
Abscess from anterior sinus infections may cause eyelid redness, swelling, and tenderness. Ethmoid sinusitis-associated abscesses often predominantly affect the medial canthus and may cause proptosis and lateral displacement of the eye if the abscess is large. Maxillary sinusitis-associated abscesses typically involve the lower eyelid and cause upward displacement of the eye. Frontal sinusitis-associated abscesses primarily affect the upper eyelid and displace the eye downward.
Abscess from posterior sinus infections mainly manifests as inflammation within deep orbital tissues, including symptoms such as vision loss, proptosis, and impaired eye movement. Eyelid symptoms are less pronounced. In sphenoid sinusitis, the infection may involve the optic canal and superior orbital fissure, leading to orbital apex syndrome, which includes symptoms such as sensory disturbances in the periorbital skin, ptosis, fixed eye position due to ophthalmoplegia, diplopia, and vision loss.
Subperiosteal orbital abscesses are often associated with significant systemic symptoms. If treated promptly, the abscess may remain localized beneath the periosteum and resolve. Alternatively, spontaneous rupture through the orbital septum with drainage through the eyelid may facilitate recovery. However, in patients with weakened immunity or delayed treatment, the abscess may rupture through the periosteum, spreading into the orbital cavity and causing orbital cellulitis.
Orbital Cellulitis and Orbital Abscess (Orbital Infections)
These represent severe rhinogenic orbital complications. Symptoms include pronounced proptosis, restricted eye movement, significant vision loss, chemosis (conjunctival edema), and severe pain in the deep orbit. Systemic symptoms such as high fever and leukocytosis are often present. In cases where the infection spreads to the eyeball, panophthalmitis may develop, leading to blindness. Further spread of inflammation through the orbital venous system can result in intracranial complications such as cavernous sinus thrombophlebitis.
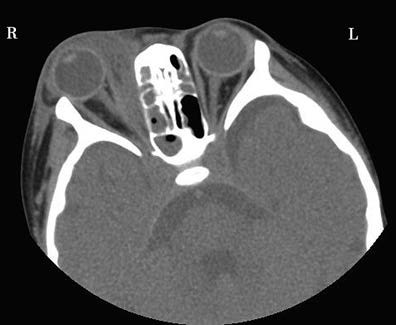
Figure 2 CT of right orbital cellulitis (horizontal view)

Figure 3 Right orbital abscess
Retrobulbar Neuritis (Inflammation of the Optic Nerve)
Inflammatory conditions of the sphenoid sinus or posterior ethmoid sinuses can cause inflammation of the retrobulbar or canalicular segments of the optic nerve. The thin or incomplete lateral wall of the sphenoid and posterior ethmoid sinuses, forming part of the medial wall of the orbital apex and optic canal, provides the anatomical basis for the optic nerve's susceptibility to these inflammatory conditions. Symptoms include severe deep orbital pain and sudden vision loss, sometimes progressing to blindness.
Diagnosis
The diagnosis is based on the history, symptoms, and signs of acute or chronic sinusitis, along with findings from sinus imaging and clinical features involving the eyes.
Orbital complications associated with acute ethmoid sinusitis in children need differentiation from acute dacryocystitis. Retrobulbar neuritis typically presents with isolated vision decline or blindness, in which case patients often first seek consultation in ophthalmology, and the underlying sinusitis may be overlooked. Thus, recurrent retrobulbar neuritis of unknown cause or neuritis unresponsive to conventional therapies warrants consideration of rhinogenic retrobulbar neuritis. Sinus CT scans are helpful for diagnosis.
Treatment
Treatment Principles
The principles of treatment involve early and active management, including anti-infective and anti-inflammatory therapy, along with ensuring unobstructed drainage of the nasal cavity and paranasal sinuses. For cases with abscess formation, incision and drainage are required. Sinus surgery or orbital decompression may be necessary, with ophthalmologists providing collaborative care when indicated.
Treatment for Periorbital Cellulitis and Subperiosteal Orbital Abscess
Management primarily focuses on treating the underlying acute sinusitis. Once an abscess has formed, it should be drained through surgical incision, alongside systemic anti-infective therapy and measures to improve sinus ventilation and drainage.
Treatment for Orbital Cellulitis and Orbital Abscess
Sinus surgery should be performed promptly, with wide incision of the orbital periosteum to facilitate drainage. Systemic anti-infective and anti-inflammatory therapies should also be intensified.
Treatment for Rhinogenic Retrobulbar Neuritis
Early sphenoidotomy and ethmoidectomy are necessary for effective management. In severe cases, optic nerve decompression is additionally required.
Perioperative management includes systemic use of antibiotics, corticosteroids, and neurotrophic agents to control infection, reduce inflammatory edema of the optic nerve, and support its recovery.
The aforementioned orbital complications may progress or transform into one another. The degree of proptosis and vision loss can serve as important indicators for assessing disease progression.