Nasal polyps originate from the bilateral middle meatus and the mucosa of the paranasal sinuses, extending into the nasal cavity and sinus chambers. They appear as smooth, translucent, soft-tissue growths. Due to the inflammatory nature of nasal polyps, the condition is clinically classified as chronic rhinosinusitis with nasal polyps (CRSwNP). Allergic fungal rhinosinusitis represents an immune response of the nasal mucosa to fungi and may also be accompanied by polyp-like structures. However, polyp-like structures associated with genetically driven conditions, such as immotile cilia syndrome or cystic fibrosis, are not discussed in this section.
Pathology
The epithelium of nasal polyp tissue primarily consists of pseudostratified ciliated columnar epithelium, accompanied by goblet cell hyperplasia, squamous metaplasia, and thickened basement membranes. The subepithelial lamina propria shows predominant edema with varying degrees of collagen fiber deposition. Eosinophils are the primary inflammatory cells, alongside infiltration by neutrophils, plasma cells, lymphocytes, mast cells, and other immune-inflammatory cells.
The histopathological features and types of inflammatory cell infiltration in CRSwNP vary by ethnicity and region. In Caucasian populations, CRSwNP is primarily characterized by Type 2 inflammation mediated by eosinophilic inflammation, with a high comorbidity rate of asthma. In contrast, approximately 50% of CRSwNP cases in East Asian countries (including China, South Korea, and Japan) exhibit non-eosinophilic inflammation with a lower asthma comorbidity rate. Based on these findings, researchers have proposed the concept of CRS endotypes, suggesting classification according to the immunopathological features of the sinus mucosa. One representative proposal involves classification based on the degree of eosinophilic infiltration in tissues, though no standardized classification criteria currently exist. Comparatively, eosinophilic CRSwNP demonstrates more significant inflammatory cell infiltration, more pronounced edema, and Type 2 inflammatory polarization, with elevated levels of IL-4, IL-5, IL-13, and IgE. Non-eosinophilic CRSwNP, on the other hand, has a greater number of glands and shows more prominent neutrophilic infiltration.
Pathogenesis
The pathogenesis of CRSwNP remains unclear, involving interactions among pathogens, genetic factors, immune mechanisms, and tissue remodeling.
Microbial Pathogens
Viruses
In vitro studies have shown that rhinoviruses can damage the epithelial barrier of the nasal mucosa, allowing pathogens to invade. Additionally, nasal polyp tissue exhibits immune deficiencies against viruses, leading to secondary inflammatory factor expression following viral infection.
Bacteria
The role of bacteria in the pathogenesis of chronic rhinosinusitis remains unresolved. Some studies have shown no significant differences in bacterial culture results between nasal mucosa from CRSwNP, CRSsNP, and healthy controls. However, other studies have reported a significantly higher positivity rate for Staphylococcus aureus in CRSwNP, particularly among Caucasian patients. Recent findings have also indicated an increasing trend of S. aureus infections in Asian populations. The distribution of bacterial species in the nasal mucosa may relate to immune differentiation. Bacterial biofilms may also play a role in CRS pathogenesis. Biofilms are bacterial communities that form under unfavorable growth conditions (e.g., nutrient or metal ion scarcity, particularly iron ions) by producing extracellular polysaccharide matrices that promote bacterial adhesion. Biofilms enhance bacterial resistance to host defense mechanisms and antibiotics, while their continuous bacterial release can act as a "bacterial reservoir" triggering acute systemic infections. The role of the microbiome in CRS is still under investigation, with evidence suggesting altered bacterial abundance and diversity in CRS.
Staphylococcus aureus Superantigens
Superantigens refer to bacterial, viral, and fungal protein exotoxins (20–30 kDa) that can activate T lymphocytes without antigen-presenting cells (APCs). They accomplish this by simultaneously binding to the α-chain of major histocompatibility complex (MHC) class II molecules on APCs and the β variable region (Vβ) of T-cell receptors (TCRs). Typically, an antigen can activate less than 0.01% of lymphocytes, whereas superantigens can activate over 30% of T lymphocytes. Superantigens also act as classical antigens, inducing antibody production and stimulating B lymphocytes to produce IgE antibodies. Common bacterial superantigens include Staphylococcus aureus toxins, such as staphylococcal enterotoxins (SEs, e.g., SEA, SEB) and toxic shock syndrome toxin-1 (TSST-1). Bachert et al. demonstrated the presence of S. aureus superantigen-specific IgE in over 50% of nasal polyp tissue homogenates, suggesting a role for SEs in the pathogenesis of nasal polyps. In vitro studies have shown that SEs can stimulate nasal polyp tissue to release IL-13, IL-5, interferon-γ (IFN-γ), tumor necrosis factor-α (TNF-α), IL-1β, and other Type 1, Type 2, and pro-inflammatory cytokines.
Fungi
Randomized double-blind placebo-controlled studies have revealed that nasal irrigation with the antifungal agent amphotericin B for three months does not alleviate symptoms of CRS, with or without nasal polyps, nor does it reduce nasal polyp scores. These findings suggest that fungi may not play a significant role in the pathogenesis of CRSwNP.
Immune Mechanisms
Epithelial Dysfunction
Tight junctions (TJs) and adherens junctions (AJs) connect epithelial cells, while desmosomes anchor columnar epithelial cells to basal cells and basal cells to the basement membrane. Studies have found that expression of TJs, AJs, and desmosomes is significantly downregulated in CRSwNP compared with controls. Some epithelial cells lose their original characteristics, becoming spindle-shaped mesenchymal cells that migrate into the subepithelial lamina propria, a phenomenon known as epithelial-to-mesenchymal transition (EMT). In EMT, the expression of TJs (e.g., ZO-1, claudins, occludin) and AJs (e.g., E-cadherin) is markedly downregulated, while these cells begin to produce collagens (types I, III, and IV), other extracellular matrix (ECM) proteins (e.g., periostin, desmin, fibronectin, tenascin, laminin, elastin), and matrix metalloproteinases (MMPs). Enzymes in allergens can disrupt TJs, and hypoxia may induce EMT. Hypoxia-inducible factor-1α (HIF-1α) has been associated with the downregulation of E-cadherin and upregulation of matrix protein α-SMA in nasal polyps. Elevated levels of IL-13 and IL-4, which are upregulated in eosinophilic nasal polyps, may also induce EMT. Studies have shown that during the initial stages of nasal polyp formation, EMT is more pronounced and is accompanied by eosinophilic inflammation and collagen deposition. Additionally, smoking has been implicated in triggering EMT in CRS.
Innate and Adaptive Immunity
When nasal epithelial cells are damaged by external factors such as microorganisms, they can produce thymic stromal lymphopoietin (TSLP), IL-33, and IL-25. These cytokines induce type 2 cytokines, such as IL-5 and IL-13, which are markedly upregulated by type 2 innate lymphoid cells (ILC2s). Unlike T and B lymphocytes, ILC2s do not require activation by antigen-presenting cells (APCs). Studies have reported increased expression of ILC2s in nasal polyp tissues.
Additionally, epithelial damage can expose pathogen-associated molecular patterns and other antigens that cross the epithelium, activating specific T and B lymphocytes. Meanwhile, type 2 cytokines produced by ILC2s can activate endothelial cells, promote adhesion molecule expression, induce chemokines, and generate factors that regulate T lymphocyte differentiation, thereby modulating adaptive immunity.
Beyond T lymphocytes, B lymphocytes also play a significant role in CRSwNP. Studies have identified increased numbers of B lymphocytes, plasmablasts, and plasma cells in nasal polyp tissues, as well as evidence of local activation, proliferation, differentiation, and upregulated antibody production. Some studies have also detected local autoantibodies targeting the basement membrane in nasal polyps, potentially associated with complement activation in the local tissue.
Tissue Remodeling
Changes in the composition of epithelial cells, alterations in the basement membrane, and either fibrosis or edema in the subepithelial lamina propria are key features of tissue remodeling. In nasal polyps, epithelial hyperplasia, an increased number of goblet cells, and thickened basement membranes are observed. The lamina propria is typically characterized by predominant edema, although some nasal polyps may exhibit substantial collagen deposition.
In general, compared with normal nasal mucosa, nasal polyps show downregulation of transforming growth factor-β (TGF-β), which suggests that edema is more dominant than fibrosis. Additionally, multiple MMPs, including MMP-7, MMP-8, and MMP-9, are significantly upregulated in nasal polyp tissues. These changes in MMP expression are closely related to changes in the ECM composition of nasal polyps.
Other Factors
The incidence of asthma in CRSwNP is significantly higher than in CRSsNP, and nasal mucosal abnormalities on CT imaging of the sinuses are seen in nearly all patients with steroid-dependent asthma. Aspirin-exacerbated respiratory disease (AERD) is a triad condition involving nasal polyps, asthma, and aspirin intolerance. Smoking may also contribute to CRSwNP by modulating immune responses.
Additionally, genetic factors may play a role. The CFTR gene, associated with cystic fibrosis, has been implicated in a subset of CRSwNP patients. Studies have also identified specific single nucleotide polymorphisms linked to CRSwNP.
Clinical Presentation
Primary Symptoms
Bilateral progressive nasal obstruction is often accompanied by clear or viscous nasal discharge. Some patients may also experience hyposmia and a sensation of facial pressure or heaviness.
Physical Signs
Anterior rhinoscopy or nasal endoscopy may reveal nasal polyps originating from the mucosa of the bilateral middle turbinates or middle meatus. Nasal polyps may also be observed in the nasal septal mucosa of the olfactory cleft, as well as the superior meatus and posterior ethmoid mucosa.
Imaging Studies
Computed tomography (CT) scanning of the paranasal sinuses is the primary imaging method but is not a mandatory diagnostic criterion. CT scans can show the extent of sinus involvement, the severity of mucosal lesions in the nasal cavity and sinuses, nasal septal deviation, and anatomical variations related to the paranasal sinuses. Certain CT features may indirectly indicate the type of inflammation present in the sinus mucosa. Magnetic resonance imaging (MRI) of the sinuses is generally not used for diagnosing CRS.
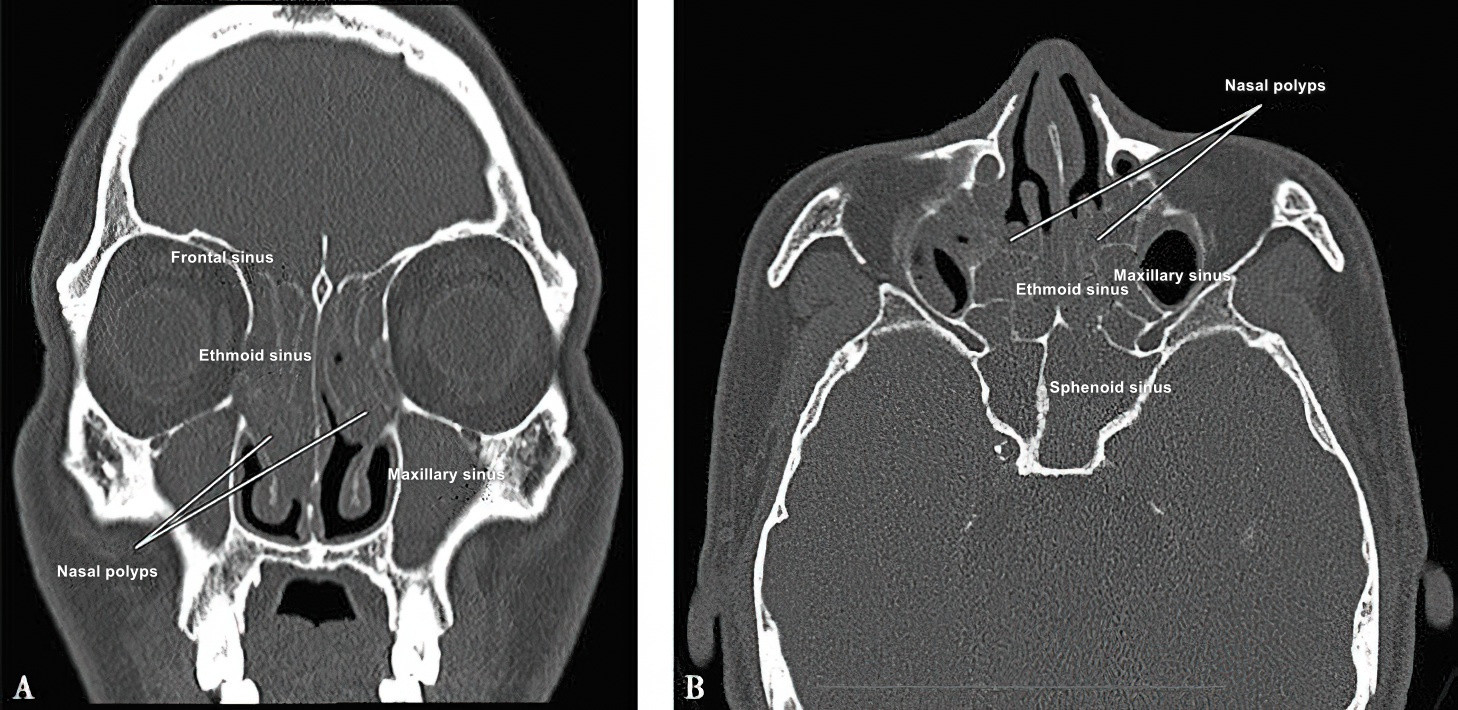
Figure 1 CT scan showing bilateral pansinusitis with nasal polyps
A. Coronal view; B. Axial view.
Diagnosis
The diagnosis involves three main components: symptoms, physical signs, and imaging studies.
Subjective assessment of the disease severity is similar to CRSsNP and can be conducted using tools like the Visual Analog Scale (VAS) or the Sino-Nasal Outcome Test (SNOT-22). Psychophysical methods are frequently used to evaluate olfactory dysfunction, with the Sniffin’ Sticks test and the University of Pennsylvania Smell Identification Test being the most common.
Nasal endoscopic evaluation is quantified using the Lund-Kennedy scoring system. Internationally, the Nasal Polyp Score (NPS) system is widely used for objective assessment of polyp size. The extent of the lesion can be evaluated using the Lund-Mackay scoring system for sinus CT scans, which is an important measure for assessing disease severity.
CRSwNP is frequently associated with localized or systemic conditions, such as adenoid hypertrophy, tonsillar hypertrophy, asthma, or genetic disorders. It is important to evaluate the patient's history of aspirin-induced asthma to exclude aspirin-exacerbated respiratory disease (AERD). For patients suspected of having asthma alongside CRSwNP, pulmonary function testing is required to prevent intraoperative asthma exacerbations. In cases of recurrent CRSwNP, nasal secretion smears can be performed preoperatively. In addition, preoperative nasal polyp biopsies may be necessary to evaluate eosinophilic and other inflammatory cell infiltration to determine the type of inflammation associated with CRSwNP.
Treatment
The treatment of CRSwNP involves medication and surgical interventions.
Medical Treatment
Local Corticosteroids
These include corticosteroid nasal sprays and nasal drops.
Mild CRSwNP
Treatment begins with local corticosteroid nasal sprays for three months. If symptoms and signs improve, the treatment is continued for an additional six months. If there is no significant improvement, surgical intervention may be considered. Alternatively, an increased dosage of corticosteroid nasal sprays or the use of nasal drops may be tried. If medical therapy remains ineffective, surgery is performed.
Moderate CRSwNP
Increased dosage of corticosteroid nasal sprays or the use of nasal drops is recommended. If the treatment is effective after three months, it can be continued for another six months. If no effect is observed, surgery is considered.
Severe CRSwNP
A combination of local corticosteroids and short-term oral corticosteroids is used. If symptoms improve after one month, nasal corticosteroid treatment is continued for an additional three to six months. If there is no improvement, surgery is considered. Postoperative long-term regular use of local corticosteroids is necessary to control postoperative inflammation and prevent or delay recurrence.
Studies have demonstrated that long-term use of local corticosteroids does not lead to atrophy of the nasal mucosa and is considered safe. Additionally, there are no contraindications for using intranasal corticosteroids in cases of viral infection or acute exacerbation of chronic rhinosinusitis. Extensive research has confirmed the efficacy of intranasal corticosteroids in treating eosinophilic nasal polyps. For many patients with nasal polyps, topical corticosteroid therapy may be sufficient to control symptoms. When combined with postoperative surgical treatment, it can significantly reduce the recurrence of nasal polyps.
Systemic Corticosteroids
Systemic corticosteroids are generally limited to the perioperative period, with a daily dose of 20–30 mg and a total treatment course typically not exceeding two weeks. They can significantly reduce the size of nasal polyps and alleviate symptoms, particularly in eosinophilic CRSwNP and CRSwNP positive for type 2 cytokines such as IL-5. However, potential side effects must be considered, including osteoporosis, abnormalities in glucose and lipid metabolism, alterations in the hypothalamic-pituitary-adrenal axis, and impacts on the cardiovascular system. Preventive measures and regular monitoring are advised.
Antibiotics
During acute infections associated with CRSwNP, antibiotic treatment can be administered based on the results of bacterial culture and sensitivity testing. Courses of treatment generally do not exceed two weeks.
Mucolytic Agents
Mucolytics can thin nasal and sinus secretions, improve ciliary activity in the nasal mucosa, facilitate mucous clearance, and support the recovery of nasal and sinus physiological functions.
Antiallergic Medications
For patients with comorbid allergic rhinitis and/or asthma, antiallergic medications can be utilized. These include oral or intranasal antihistamines and oral leukotriene receptor antagonists, with treatment lasting no less than four weeks. In patients with asthma, oral leukotriene receptor antagonists are preferred.
Nasal Irrigation
Nasal irrigation is a frequently employed adjunctive therapy, particularly following endoscopic nasal surgery.
Biologic Treatments
Multiple global multicenter randomized controlled trials have demonstrated that subcutaneous injection of monoclonal antibodies targeting IgE, IL-5, or the IL-4 receptor can significantly reduce the size of nasal polyps, relieve symptoms such as nasal obstruction and rhinorrhea, improve olfactory function, and enhance quality of life. These therapies are specifically directed toward corresponding immunological characteristics and subtypes, representing a future option for precision medicine. Certain biologics have already been approved in Europe and the United States for the treatment of refractory severe CRSwNP, reducing the need for repeated surgeries or prolonged use of systemic corticosteroids in these patients.
Surgical Treatment
When medical treatment proves ineffective, surgical intervention can be considered. Under nasal endoscopy and television monitoring, specialized surgical instruments and powered equipment are used to remove nasal polyps, open the sinuses, and improve ventilation and drainage. Detailed information on surgical techniques is described in Endoscopic Nasal Surgery Techniques.
Functional endoscopic sinus surgery (FESS) is performed in nasal endoscopy and television guidance to remove nasal polyps, open the sinuses, and address anatomical abnormalities such as nasal septal deviation and concha bullosa. Efforts are made to preserve the sinus mucosa as much as possible, reconstruct normal ventilation and drainage pathways in the nasal cavity and sinuses, and promote the resolution of mucosal inflammation. However, postoperative use of intranasal corticosteroids is necessary to maintain these outcomes.