Etiology
Chronic rhinosinusitis without nasal polyps (CRSsNP) arises due to a combination of anatomical abnormalities, genetic predisposition, and environmental factors.
Microbial Factors
Bacterial Factors
The use of bacterial 16sRNA-based metagenomic sequencing technology has revealed that disruptions in bacterial communities may be associated with the pathogenesis, inflammatory state, and treatment outcomes of CRS. Clinical studies indicate that conventional antibiotic therapy often yields poor results, and it is challenging to distinguish between bacterial infection and colonization. The association between CRSsNP and bacterial infection is not significant, suggesting that bacterial infection alone may not be a direct causative factor for CRSsNP. However, bacteria may induce mucosal inflammation in the nasal cavity and sinuses through alternate pathways. Research into bacterial biofilms, which are protective polymeric structures produced by bacteria under unfavorable environmental conditions, has demonstrated their role in shielding bacteria from host immune defenses and antibiotics. Beyond serving as pathogenic agents, bacterial biofilms can act as antigens, superantigens (e.g., Staphylococcus superantigens), adjuvants, toxins, or inflammatory mediators, contributing to the onset and progression of CRSsNP. Thus, bacterial biofilms are critical factors influencing drug resistance and poor treatment efficacy in CRSsNP.
Fungal Factors
Fungal cultures are commonly identified in the nasal secretions of CRSsNP patients, but direct evidence linking fungi to the causation of CRSsNP remains lacking. Some studies suggest that fungi might induce an inflammatory response, leading to epithelial damage and subsequent bacterial colonization, contributing to CRSsNP. However, multiple prospective, randomized, double-blind trials have failed to demonstrate the efficacy of antifungal agents in treating CRSsNP, leaving the role of fungi in its pathogenesis unclear.
Viral Factors
Studies have shown a significantly higher detection rate of rhinoviruses in CRSsNP patients compared to healthy controls. Viruses may disrupt the mucosal epithelial barrier of the upper respiratory tract and could play a role in the development of CRSsNP.
Local Factors
Ciliary Dysfunction
Proper ciliary function in the nasal and sinus mucosa is essential for maintaining mucosal cleanliness and preventing chronic inflammation. Dysfunction of the mucociliary system may be primary or secondary. Research indicates that CRSsNP patients often develop secondary ciliary motility impairments due to epithelial damage in the nasal and sinus regions. This secondary dysfunction is typically reversible as inflammation and infection resolve. Primary ciliary dyskinesia, an autosomal recessive genetic disorder characterized by the absence of central microtubular structures in cilia, leads to impaired ciliary movement. This condition is often associated with CRSsNP, respiratory tract diseases, and infertility. When combined with organ situs anomalies, it is known as primary ciliary dyskinesia syndrome.
Anatomical Abnormalities
Local anatomical deviations, such as concha bullosa, nasal septal deviation, or abnormalities in the location or structure of the uncinate process, may impair ventilation and drainage in the ostiomeatal complex, acting as potential risk factors for CRSsNP. However, some studies suggest that local anatomical abnormalities are not directly causal for CRSsNP.
Epithelial Barrier Disruption
Damage and necrosis of epithelial cells leading to mucosal lamina propria protrusion and tissue repair may play a significant role in the onset of CRSsNP. Disruption of tight junction integrity in epithelial cells, along with reduced expression of host defensive molecules, may weaken the body's defense against microbial infections and impair the development of an effective adaptive immune response. Damaged epithelial cells can secrete thymic stromal lymphopoietin (TSLP), interleukin-25 (IL-25), and IL-33, which may directly activate type 2 innate lymphoid cells (ILC2s) to induce eosinophilic inflammation or act on dendritic cells to trigger a Th2 immune response.
Systemic Factors
Allergic Reactions
Epidemiological data indicate an increased prevalence of allergic rhinitis among CRSsNP patients. However, the influence of allergic rhinitis on the development of CRSsNP remains unclear, with no direct evidence suggesting that allergies are a primary or immediate causative factor. Allergic rhinitis and CRS may coexist as comorbid conditions rather than having a causal relationship. Allergic rhinitis may affect the inflammatory response in CRSsNP, where allergen-induced mucosal swelling can lead to sinus obstruction, poor ventilation, mucus retention, and subsequent infection. CRSsNP cases with comorbid allergic rhinitis may exhibit distinct histopathological characteristics.
Immune Deficiency
Immune deficiency constitutes a predisposing factor for CRSsNP. Patients with immune deficiency-related CRSsNP often experience frequent recurrences and may also suffer from infections in other organ systems.
Other Factors
Odontogenic Diseases
Chronic maxillary sinusitis can result from apical infections of teeth that extend into the maxillary sinus, with anaerobic bacteria being the predominant pathogens.
Helicobacter Pylori Infection and Gastroesophageal Reflux Disease (GERD)
Helicobacter pylori DNA has been detected in the tissues of CRSsNP patients. Studies have also reported that some children with refractory CRSsNP exhibit symptoms of acid reflux, with symptomatic improvement following antacid therapy.
Pathology
The primary pathological features include inflammatory cell infiltration, tissue edema, collagen deposition, mucous gland hyperplasia, and squamous epithelial metaplasia. In some patients, significant fibrosis, vascular proliferation, and edema are observed. The infiltrating inflammatory cells mainly consist of lymphocytes (T cells and B cells), plasma cells, macrophages, mast cells, dendritic cells, neutrophils, and eosinophils. T lymphocyte infiltration predominantly involves CD8+ cells.
CRSsNP can be classified into eosinophilic and non-eosinophilic subtypes. Unlike Western populations, most CRSsNP cases exhibit non-eosinophilic inflammation. Compared with chronic rhinosinusitis with nasal polyps (CRSwNP), CRSsNP is characterized by relatively lower levels of total inflammatory cell infiltration, eosinophils, plasma cells, CD8+ T cells, B cells, and macrophages. However, it shows more significant neutrophilic infiltration, collagen deposition, and an increase in the number of mucosal glands.
Clinical Manifestations
Nasal Obstruction
Nasal obstruction is one of the primary symptoms and often results from thickened nasal and sinus mucosa or reactive swelling of the turbinates.
Nasal Discharge
Another main symptom is mucopurulent nasal discharge, which may be accompanied by postnasal drip. Odontogenic maxillary sinusitis commonly presents with a foul odor.
Facial Pressure or Pain
Considered a secondary symptom, it typically manifests as generalized facial pressure or pain, with a sense of compression, and may aid in identifying the affected side.
Olfactory Dysfunction
This secondary symptom ranges from temporary to permanent loss or reduction of the sense of smell.
Other Symptoms
General symptoms may include fatigue, coughing, and other systemic manifestations.
Examinations
Signs
Anterior rhinoscopy or nasal endoscopy may reveal mucous or mucopurulent secretions originating from the middle meatus and olfactory cleft, along with nasal mucosal congestion and edema.
Auxiliary Examinations
Sinus computed tomography (CT) imaging may show inflammatory changes in the mucosa of the sinus or the ostiomeatal complex. The Lund-Mackay scoring system is recommended for grading sinus CT findings.
Sinus CT is not deemed essential for diagnosis. Magnetic resonance imaging (MRI) can provide detailed information on the extent, nature, and anatomical relationships of soft tissue lesions within the nasal cavity and sinuses, offering valuable insights for differential diagnosis, though it is also not mandatory for diagnosis.
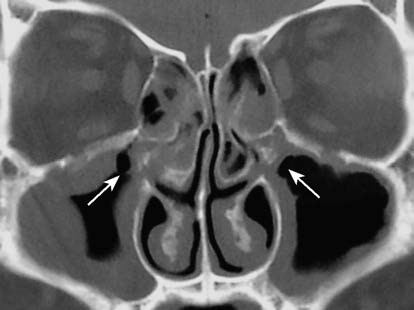
Figure 1 CT showing obstruction of the ostiomeatal complex
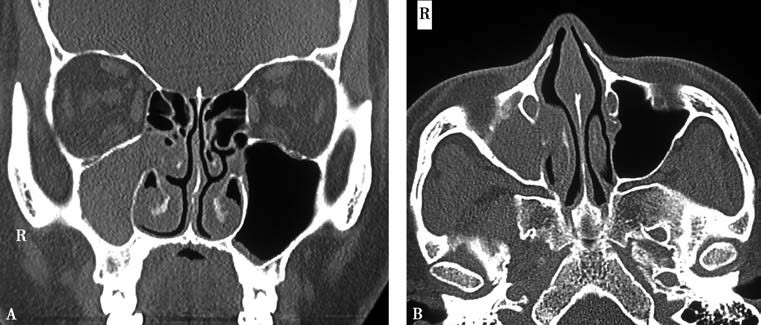
Figure 2 Right maxillary sinusitis
A. Coronal view of sinus CT showing right maxillary sinusitis.
B. Axial view of sinus CT showing right maxillary sinusitis.
Diagnosis
The diagnosis of CRSsNP mainly relies on symptoms, physical signs, and/or sinus CT imaging. In children, the diagnosis should prioritize clinical symptoms and findings from nasal endoscopy, with careful consideration of indications for sinus CT.
Key Symptoms
Primary Symptoms: Nasal obstruction and mucous or mucopurulent nasal discharge.
Secondary Symptoms: Facial pressure or pain, and reduction or loss of olfactory function.
Diagnosis requires the presence of at least two or more of the above symptoms, with at least one primary symptom (nasal obstruction or mucous/mucopurulent nasal discharge). The disease must persist for more than 12 weeks.
The severity of the disease can be quantified using the Visual Analogue Scale (VAS), with scores categorized as mild (0–3), moderate (>3–7), or severe (>7–10). A VAS score greater than 5 indicates a significant impact on the patient's quality of life. Additionally, the Sino-Nasal Outcome Test-22 (SNOT-22) scale may be used for evaluation.
Treatment
Treatment Strategy
Pharmacological therapy is regarded as the first-line approach. A combination of intranasal corticosteroids and nasal irrigation is recommended for a duration of three months. If the treatment response is insufficient, endoscopic sinus surgery may be considered. Postoperative care should include regular follow-up and the continued use of intranasal corticosteroids combined with nasal irrigation.
For some refractory patients, individualized treatment with low-dose macrolide antibiotics may be prescribed based on the patient’s specific condition.
In cases of complications, such as periorbital swelling, globe displacement, diplopia, vision loss, ophthalmoplegia, severe frontal headache, frontal swelling, meningitis, or focal neurological deficits, the underlying cause should be identified promptly, and surgical intervention may be necessary when appropriate.
Pharmacological Treatment
Glucocorticoids
Glucocorticoids possess potent anti-inflammatory and immunosuppressive properties and represent the most crucial class of drugs for treating chronic rhinosinusitis (CRS). Intranasal sprays are the most commonly used formulation in clinical practice. Intranasal glucocorticoids are recommended as the first-line treatment for CRS, with a treatment duration of no less than 12 weeks. Preoperative use of glucocorticoids has been shown to alleviate symptoms, reduce intraoperative bleeding, improve surgical field quality scores, and shorten surgical time. Postoperative use, while not improving symptoms, can enhance endoscopic scores and reduce recurrence rates. Local side effects of glucocorticoids include nasal bleeding, dryness, septal perforation, burning sensations, and irritation, although these occur infrequently and show no significant difference compared to placebo. A long-term and sustained use of intranasal glucocorticoids (over 12 weeks) is necessary to maintain efficacy, and these agents do not provide rapid symptom relief or immediate reduction of mucosal inflammation, which is a limitation in clinical applications.
In addition to sprays, other local delivery methods, such as drops, nasal irrigation, and nebulized inhalation, are also utilized in clinical practice. Nebulized inhalation of glucocorticoids provides a safe and effective alternative to conventional intranasal sprays and systemic oral glucocorticoids for CRS management. Systemic oral glucocorticoids are generally not recommended for treating CRSsNP.
Nasal Irrigation
Nasal irrigation is an effective treatment for CRSsNP and is also commonly employed as an adjunct therapy following endoscopic sinus surgery.
Antibiotics
Antibiotics are primarily used during acute exacerbations of CRSsNP and to manage postoperative infections following endoscopic sinus surgery.
Other Medications
For patients with severe nasal obstruction, short-term use of decongestants may be considered, with a duration not exceeding one week. For patients with concurrent allergic rhinitis or bronchial asthma, antiallergic medications, such as antihistamines and leukotriene receptor antagonists, may be used. Proton pump inhibitors or newer potassium-competitive acid blockers can be prescribed for patients with gastroesophageal reflux disease to manage acid suppression.
Endoscopic Sinus Surgery
Endoscopic sinus surgery may be considered for patients who do not respond to standardized pharmacological treatment, present with significant anatomical abnormalities, or develop intracranial or orbital complications. Strict criteria should be applied to determine surgical indications in pediatric patients, and surgery generally should not be performed in children under the age of 12.
Surgical treatment requires not only the surgeon's expertise but also a coordinated regimen of preoperative and postoperative medications along with regular follow-up care. Preoperative local medication is utilized to minimize nasal and sinus mucosal inflammation. The objectives of endoscopic sinus surgery include restoring patency of the ostiomeatal complex, correcting anatomical abnormalities in the nasal cavity, removing irreversible pathological lesions, and preserving as much healthy nasal and sinus mucosa as possible to restore ventilation and drainage.
Postoperative care involves regular follow-up and comprehensive pharmacological therapy for at least 12 weeks. Postoperative endoscopic examination and cavity cleaning are typically performed for a duration of 3 to 6 months.
Environmental Control
Elimination of potential triggers or predisposing factors is emphasized, such as smoking cessation, use of air filtration systems, and avoidance of allergens.