Acute rhinitis refers to an acute inflammatory condition of the nasal mucosa caused by viral infection. It is part of an upper respiratory tract infection and can occur throughout the year, with increased susceptibility during seasonal transitions, particularly in winter. The condition commonly referred to as the "common cold" often involves acute rhinitis as part of the clinical presentation.
Etiology
The primary cause of acute rhinitis is viral infection, often accompanied by secondary bacterial infection. Rhinoviruses are the most common pathogens, followed by influenza and parainfluenza viruses, adenoviruses, coronaviruses, coxsackieviruses, respiratory syncytial virus, echoviruses, as well as orthomyxoviruses and paramyxoviruses.
The primary mode of viral transmission is through inhalation via the respiratory tract, followed by entry through contaminated objects or food. Factors that reduce the body’s resistance can predispose the nasal mucosa to viral invasion. Common contributing factors include:
- Systemic Factors: Cold exposure, overexertion, excessive smoking or alcohol consumption, vitamin deficiencies, endocrine imbalances, or other chronic systemic diseases (e.g., heart, liver, kidney disorders).
- Local Factors: Chronic nasal conditions such as deviated nasal septum, chronic rhinitis, nasal polyps, as well as infections in adjacent areas, including chronic sinusitis and purulent tonsillitis.
Pathology
Early-stage changes include vascular spasm, mucosal ischemia, and reduced glandular secretion. This progresses to vascular dilation, mucosal hyperemia, edema, increased glandular secretion, and infiltration of submucosal monocytes and macrophages. In cases with secondary bacterial infection, submucosal neutrophil infiltration, as well as necrosis and shedding of cilia and epithelial cells, may occur. During the recovery phase, regeneration of epithelial and ciliated cells occurs, with gradual restoration of ciliary function and normal morphology.
Clinical Manifestations
Symptoms
Early symptoms include nasal dryness, burning sensation, itching, soreness or discomfort, and sneezing. These progress to nasal congestion, watery nasal discharge, reduced sense of smell, and a muffled nasal voice. With secondary bacterial infection, nasal discharge becomes viscous, mucoid-purulent, or purulent. Ear-related symptoms such as fullness or blockage may occur, and some patients may experience tinnitus or hearing loss.
Systemic symptoms vary among individuals and may range in severity. Early systemic manifestations typically include general discomfort, fatigue, headache, and fever (37–38°C) resembling a "common cold." In children, systemic symptoms tend to be more pronounced, often presenting with high fever (above 39°C), convulsions, and digestive symptoms such as vomiting and diarrhea.
Signs
Nasal mucosa exhibits congestion and swelling, with significant hyperemia and engorgement of the inferior turbinate. The nasal cavity and nasal floor contain secretions that are initially watery but gradually become viscous, mucoid-purulent, or purulent.
The incubation period typically lasts 1–3 days, and the course of the disease is approximately 7–10 days. In the absence of complications, symptoms gradually subside and resolve.
Complications
Acute Sinusitis
Acute inflammation of the nasal mucosa may spread to the sinus mucosa via the sinus ostium, leading to acute sinusitis. This often begins as catarrhal inflammation, which may progress to purulent inflammation, commonly involving the maxillary sinuses and ethmoid sinuses. Symptoms include worsening nasal congestion compared to rhinitis, purulent nasal discharge, facial or nasal root pain or discomfort, and decreased sense of smell.
Acute Otitis Media
The spread of infection to the middle ear through the eustachian tube results in inflammation. This is more common in children due to the anatomical characteristics of their eustachian tube (wider, shorter, and more horizontal). Symptoms include ear pain, a sensation of blockage, hearing loss, tinnitus, and in some cases, otorrhea.
Acute Pharyngitis, Laryngitis, Tracheitis, or Bronchitis
Infection may spread downward through the nasopharynx, causing inflammation in the throat, larynx, trachea, or bronchi. In children, the elderly, and individuals with weakened immunity, pneumonia may develop as a complication. Symptoms include throat pain, foreign body sensation, burning sensation, discomfort during swallowing, hoarseness, coughing, sputum production, and chest pain.
Nasal Vestibulitis
This uncommon complication arises from the direct spread of infection or due to increased nasal secretions. Repeated nose-blowing and the irritation of secretions may lead to inflammation of the nasal vestibule skin. Symptoms include burning pain at the nasal vestibule, dry sensations, and crust formation.
Other Infections
Rarely, infection may spread via the nasolacrimal duct, causing ocular complications such as conjunctivitis or dacryocystitis. Symptoms include conjunctival redness and swelling, excessive tearing, and a burning or uncomfortable sensation in the eyes.
Differential Diagnosis
Influenza (Flu)
Influenza presents with more severe systemic symptoms, such as high fever, chills, headache, and generalized joint and muscle pain. Symptoms like nasal congestion and rhinorrhea are relatively mild. Acute nasal mucosal inflammation can also occur as part of the pathological changes during influenza.
Allergic Rhinitis
Often misdiagnosed as acute rhinitis, allergic rhinitis is characterized by paroxysmal sneezing and watery nasal discharge accompanied by nasal and ocular itching. Symptoms tend to have a short duration, generally resolving within half a day, and normalcy is restored afterward. Allergic rhinitis often exhibits seasonal or perennial patterns, without systemic symptoms like fever. Nasal examination shows pale, edematous nasal mucosa, significant swelling of the inferior turbinates, and abundant watery nasal secretions. Diagnostic tests such as cytology of nasal secretions, specific skin prick testing (SPT), serum-specific IgE measurement, and nasal provocation tests show positive results.
Vasomotor Rhinitis
Symptoms resemble those of allergic rhinitis and also lack systemic manifestations. Triggers are often distinct and episodes tend to occur abruptly and subside quickly. Nasal examination does not show significant pallor or edema of the mucosa, and serum-specific IgE tests are negative.
Acute Infectious Diseases
Early symptoms of some respiratory infectious diseases, such as measles, scarlet fever, pertussis, and nasal diphtheria, can include acute rhinitis-like manifestations. In addition to nasal symptoms, these diseases present their distinct clinical signs, such as rashes or severe systemic symptoms like high fever, chills, headache, and generalized muscle aches. Differential diagnosis relies on thorough physical examination and close observation of the disease progression.
Prevention
Strengthening the Body’s Resistance
Regular physical exercise, outdoor activities, and adaptation to cold environments may enhance resistance to infection. Maintaining a balance between work and rest and following a healthy diet also contribute to improved immunity.
Avoiding Exposure to Infection Sources
During flu outbreaks, close contact with infected individuals should be minimized, and public places should be avoided as much as possible. Ensuring indoor ventilation helps reduce the risk of infection.
Treatment
The primary treatment approach focuses on supportive care, symptomatic relief, and addressing the underlying causes, with attention to preventing complications.
Local Therapy
Topical Nasal Decongestants
Commonly used decongestants include oxymetazoline hydrochloride nasal drops, 0.5%–1% ephedrine nasal drops (0.5% for children), and naphazoline hydrochloride nasal drops. These medications reduce nasal mucosal swelling, alleviate nasal congestion, and improve drainage. However, prolonged use of decongestants, beyond seven days, can lead to medication-induced rhinitis.
Common methods of nasal instillation include:
- Supine Position: Lying on the back with a cushion under the shoulders, the nostrils pointing upward, or with the head hanging backward over the edge of the bed.
- Sitting Position: Sitting with the back supported, head tilted back, and nostrils pointing upward.
- Lateral Position: Lying on the affected side with the head hanging over the edge of the bed, suitable for unilateral conditions.
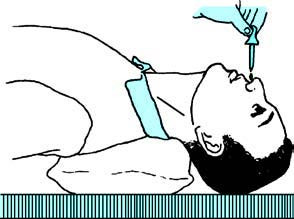
Figure 1 Supine position for nasal medication administration
After assuming the appropriate position, 2–3 drops of medication can be dropped into each nostril and the position should be maintained for 2–3 minutes. For nasal sprays, the head remains upright during administration.
Topical Nasal Corticosteroids
Nasal corticosteroids are the first-line localized treatment for rhinitis and sinusitis. They possess anti-inflammatory properties by regulating gene transcription to increase anti-inflammatory gene expression and decrease pro-inflammatory gene expression. These medications reduce inflammatory reactions in the nasal mucosa, alleviating symptoms like nasal congestion. Due to their low systemic bioavailability, they have minimal systemic side effects and are ideal for inflammatory conditions of the nasal mucosa and sinuses.
Adverse effects of nasal corticosteroids are primarily localized, such as nasal dryness, occasional nosebleeds, or exceedingly rare nasal septum perforation. Proper usage technique is crucial.
During application, the spray nozzle should face the outer side of the nasal cavity (towards the lateral canthus). Spraying the left nasal cavity with the right hand and the right nasal cavity with the left hand ensures proper direction away from the nasal septum, minimizing the risk of septal damage when used long-term.
After application, keeping the nostrils upward and inhaling deeply helps distribute the medication evenly across the nasal mucosa for optimal therapeutic effect. It is important to consider age-appropriate formulations for pediatric patients when using nasal corticosteroids.
Systemic Therapy
Treatment targets underlying causes and systemic symptoms. Antibiotics may be used in cases of bacterial infection or suspected complications. Adequate rest, hydration, a light diet, and proper bowel management also contribute to recovery.