Congenital choanal atresia is a rare nasal malformation first described by Johann George Roederer in 1755. It has a low incidence rate, occurring in approximately 1 in 5,000 to 1 in 7,000 newborns, with a unilateral to bilateral case ratio of about 1.6:1. The condition affects males and females at similar rates. Based on the extent of atresia, it may be unilateral or bilateral. Based on the tissue type involved in the atresia, it may be categorized as membranous, bony, or mixed. It may exist as an isolated congenital anomaly or in combination with other congenital defects affecting other parts of the body.
Pathogenesis
There are four main theories regarding the pathogenesis of congenital choanal atresia:
Persistence of the Buccopharyngeal or Bucconasal Membrane
During normal embryological development, the buccopharyngeal membrane ruptures around the 4th week and the buccal-nasal membrane ruptures around the 6th to 7th weeks to form the primitive choanae. Thick intervening mesenchymal tissue may hinder rupture, leading to choanal atresia.
Epithelial Plug Development
After the formation of the primitive choanae during embryonic development, one or both sides may be blocked by an epithelial plug. This plug may evolve into membranous or bony atresia.
Proliferation of Surrounding Tissue
Abnormal development of the bony choanae may result in excessive growth of the bones surrounding the choanae—including the sphenoid body and its medial pterygoid plate, the posterior margin of the vomer and its bony wings, and the horizontal plate of the palatine bone—leading to mixed atresia composed of both bony and cartilaginous components. The cartilaginous portion may originate from the palatine bone.
Abnormal Neural Crest Cell Migration:
Clinical Manifestations
Newborns rely solely on nasal breathing, so bilateral congenital choanal atresia presents immediately after birth with severe respiratory distress, cyanosis, and even potential asphyxiation or death. Symptoms improve or disappear when the infant cries due to mouth breathing but worsen during feeding or nasal breathing, causing cyanosis to recur and leading to feeding difficulties. Some infants may survive into infancy if they adapt by establishing a coordinated alternation between sucking and breathing after approximately 4 weeks. As they grow older, children may exhibit increasingly noticeable obstructive nasal speech, gelatinous nasal secretions that are difficult to expel, snoring, and symptoms of sleep apnea syndrome. They may frequently appear drowsy and lethargic. In cases of unilateral choanal atresia, infants may display difficulty breathing during feeding but may otherwise remain asymptomatic.
Diagnosis
Newborns experiencing respiratory distress, cyanosis, and feeding difficulties with symptoms improving when crying and intermittent difficulty during feeding should raise suspicion for congenital choanal atresia. Nasal endoscopy and nasal CT are frequently used for diagnosis.
Nasal Endoscopy
This allows direct evaluation of choanal atresia, determination of whether the condition is unilateral or bilateral, complete or incomplete, and aids in planning the surgical approach.
CT Examination
High-resolution CT of the nasal sinuses, incorporating coronal, axial, and sagittal views, can provide a definitive diagnosis. Both bone and soft tissue windows allow observation of the location, thickness, type, and anatomical relationships of the atretic plate.
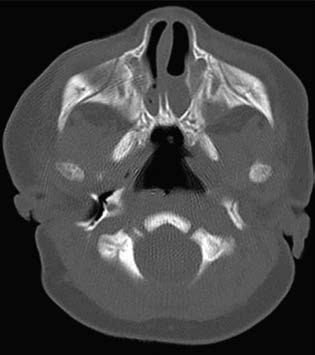
Figure 1 CT imaging of bilateral bony choanal atresia (axial view)
Treatment
Emergency Care
In cases of bilateral choanal atresia in newborns, establishing an oral airway is essential to ensure ventilation and prevent asphyxiation. Focus is also placed on nutritional support and prevention of secondary infections. A small-sized metal airway or a modified McGovern nipple (with the tip cut off) can be inserted into the oral cavity. Definitive surgery is undertaken electively.
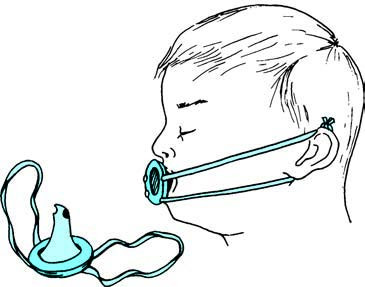
Figure 2 Diagram of the McGovern nipple
Surgery
Surgical approaches include transnasal, transpalatal, transseptal, and transmaxillary routes. The choice depends on patient age, severity of symptoms, type and thickness of the atresia, and overall health. Endoscopic surgery is commonly employed due to its clear visualization. Under general anesthesia and after nasal mucosa decongestion, a 0° nasal endoscope is inserted through the anterior naris. For membranous or mixed atresia, the choanae can be reconstructed using a cutting tool or plasma ablation, enlarging the opening to 10–12 mm and placing a silicone stent for support. For bony atresia, resection of the bony atretic plate is necessary, followed by stent placement.
Postoperative Atresia Recurrence
Recurrence may result from insufficient enlargement of the choana during surgery, inadequate mucosal flap coverage of the wound bed leading to granulation tissue proliferation, premature removal of the stent, gastroesophageal reflux, or surgery performed at an age younger than 10 days without sufficient postoperative endoscopic cleaning. Adequate enlargement of the choana during surgery, optimal placement and stabilization of the stent, and regular cleaning of the surgical site help reduce the likelihood of postoperative restenosis.