Nasal encephalocele refers to the protrusion of meninges and brain tissue through congenital cranial sutures or defects in the cranial bone into the nasal root or nasal cavity. It is most commonly observed in newborns and infants. The incidence is low, with Southeast Asia reporting higher rates compared to North America.
Etiology
During embryonic development, brain tissue herniates through unfused cranial sutures to the external cranium. Alternatively, it may result from increased intracranial pressure during delivery.
Classification
Nasal encephalocele is classified into two types based on the location of the protrusion:
- Fontanelle Type: The herniated tissue passes through the foramen cecum anterior to the crista galli of the ethmoid bone, protruding externally into the nasal region.
- Basal Type: The herniated tissue exits posterior to the crista galli, remaining within the nasal cavity.
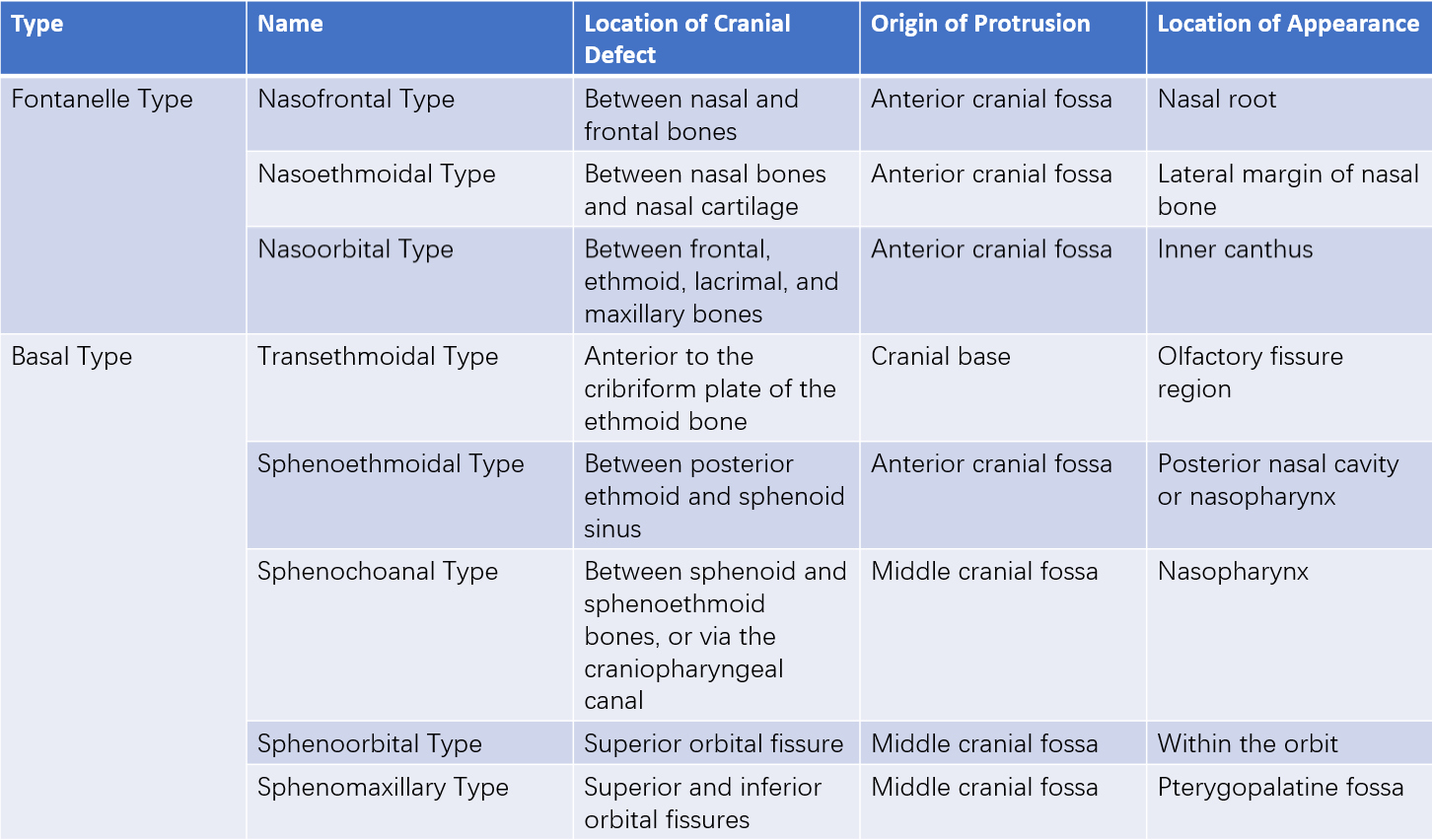
Table 1 Classification of encephalocele
Pathology
Based on the content of the protruding tissue, nasal encephalocele can be categorized into three types:
- Meningocele: In cases of mild severity, the protrusion contains only meninges and cerebrospinal fluid.
- Encephalomeningocele: In moderately severe cases, the protrusion also includes brain tissue.
- Hydroencephalocele: In the most severe cases, the herniation contains the anterior horn of a cerebral ventricle.
The histological structure of all three types typically consists of an outer layer (skin or mucosa), subcutaneous or submucosal tissue, dura mater, and cerebrospinal fluid beneath the dura.
Clinical Manifestations
Fontanelle Type (External Nasal Encephalocele)
A near-midline or slightly lateralized round mass at the nasal root is visible in newborns. The surface is smooth and has both a fluctuation and pulsation sensation upon palpation. Crying or jugular vein compression often enlarges the mass, though this may not be apparent if the cranial base defect is small. External nasal encephalocele can cause facial deformities, such as an increased interorbital distance.
Basal Type (Internal Nasal Encephalocele)
Newborns may present with unilateral nasal obstruction, with or without clear nasal discharge. Feeding difficulties may also occur. Physical examination reveals a smooth mass within the nasal cavity or nasopharynx, often positioned at the top of the nasal cavity or in the nasopharyngeal region.
Diagnosis
A soft, rounded mass above the nasal root in newborns that demonstrates positive transillumination suggests a diagnosis of fontanelle-type nasal encephalocele, which is relatively easy to identify. However, the basal type is often concealed and lacks specific clinical signs, making it prone to misdiagnosis. If a newborn has unilateral nasal obstruction, feeding difficulties, and clear nasal discharge (with or without it), along with a smooth, grayish-white, translucent mass in the nasal passage or nasopharynx, nasal encephalocele should be considered.
Imaging studies play a crucial role in diagnosing nasal encephalocele in infants. Nasal CT scans typically reveal expansile, hypodense or isodense soft tissue lesions within the nasal cavity or nasopharynx. The scans often show bone defects at the cranial base midline, although in infants with incomplete cranial base ossification or thin bone, even an intact cranial base may appear as a defect on CT. Nasal MRI typically shows a long T1 and long T2 signal within the nasal cavity or nasopharynx, continuous with the subarachnoid space. It additionally helps determine the location and extent of the herniation. Aspiration of the mass is generally avoided to prevent intracranial infection.
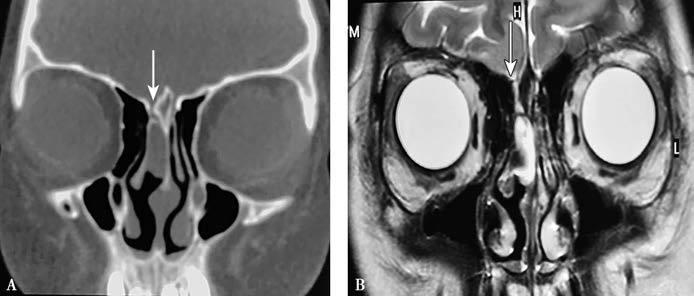
Figure 1 Imaging features of nasal encephalocele
A. Nasal CT (coronal view) demonstrates a homogeneous soft tissue density opacity at the top of the right nasal cavity with a bony defect in the cranial base adjacent to the right side of the crista galli (arrow).
B. Nasal MRI (coronal view) shows a long T2 signal intensity at the top of the right nasal cavity, continuous with the subarachnoid space (arrow).
Differential diagnosis should distinguish nasal encephalocele from nasal gliomas and nasal dermoid cysts. Nasal gliomas appear as soft tissue density masses on MRI and do not connect with the subarachnoid space. Nasal dermoid cysts present as subcutaneous nasal root masses or small pores on the nasal dorsum. Secondary infections can cause swelling and redness. MRI can assess whether the cyst communicates with the intracranial cavity, and a definitive diagnosis can be made via postoperative pathological examination.
Treatment
Once nasal encephalocele is discovered, surgery is recommended at the earliest opportunity. Contraindications for surgery include severe brain malformations, developmental abnormalities, rupture and infection of the herniation, internal nasal encephalocele with severe nasal and sinus infection, and encephalocele accompanied by hydrocephalus and brain anomalies. Surgical procedures include resection of the herniated mass and repair of the cranial bone defect. Conventional approaches primarily involve intracranial, extracranial, or combined craniofacial surgical techniques. For extensive cranial base defects or for craniofacial reconstruction with cosmetic considerations, an extracranial approach primarily handled by neurosurgery may be necessary.
In recent years, endoscopic techniques have been increasingly utilized for the treatment of nasal encephalocele, offering advantages such as improved visualization, reduced trauma, minimal bleeding, and fewer complications.