Historical Development and Pros and Cons of Endoscopic Ear Surgery
Minimally Invasive Surgical Concept
Minimally invasive surgical techniques represent a major trend in 21st-century surgery. The application of endoscopes and minimally invasive approaches has revolutionized conventional surgical methods. These techniques enable the complete removal of lesions while preserving the normal structure and function of organs to the greatest extent possible. They are associated with shorter operation times, reduced blood loss, faster patient recovery, lower rates of complications, and decreased recurrence rates.
Microscopic Ear Surgery
The surgical microscope, introduced to otologic surgery in the 1950s, provides illumination and magnification during surgery and marked the beginning of otologic microsurgery. This innovation significantly advanced the development of ear surgery and is considered a milestone in the field. However, the linear field of view offered by the microscope can result in blind spots in both the surgical field and the operative angle during middle ear surgeries. While these challenges can be largely overcome by widening the surgical approach and through surgeons' experience, the utilization of endoscopes has greatly enhanced the ease and precision of these procedures.
Endoscopes in Otology
Endoscopic techniques were first used in the 1960s to examine the external ear, middle ear, and surgical cavities. Before 1990, endoscopes were primarily diagnostic tools in otology, rarely extending beyond the tympanic membrane. In recent years, advancements in equipment, instruments, and surgical techniques—especially with the introduction of 4K high-definition and 3D wide-angle endoscopes with a diameter of 3mm—have enabled highly detailed views of ear anatomy and facilitated surgical manipulation under endoscopic guidance. These developments laid the foundation for the use of endoscopic techniques in middle ear surgeries. In recent years, endoscopic ear surgery has evolved rapidly within the fields of otology and lateral skull base surgery, gaining widespread acceptance.
Currently, endoscopes used in otology include rigid and flexible types, with rigid endoscopes being the most commonly employed. Frequently used lenses have angles of 0°, 30°, and 45°, and common diameters include 1.9mm, 2.7mm, and 3.0mm. Endoscopes can be connected to video systems, supporting 4K high-resolution imaging and 3D visualization. These features allow exceptional exposure and visualization of hidden, deep-seated structures and spaces. In contrast, achieving a similar field of view under a microscope often requires the removal of a significant amount of non-pathological tissue to expose or access these structures. Meanwhile, endoscopic ear surgery has unique anatomical, surgical approach, and technical characteristics due to its reliance on endoscopic manipulation, which has, to some extent, altered conventional perceptions and techniques in otologic surgery. The focus remains on the complete removal of pathology while preserving or restoring the physiological function of the middle ear.
Advantages of Endoscopic Ear Surgery
Endoscopic surgery, through a natural approach via the ear canal, allows for lesion removal while preserving the structure and function of the ear as much as possible. It offers numerous advantages, including excellent illumination, clear imaging, a wide field of view, three-dimensional visualization, precision, and compact instrumentation. The ability to adjust angles in real-time, focus freely, and closely observe structures contributes to reduced surgical trauma and faster postoperative recovery. These attributes demonstrate the significant advantages of endoscopic techniques in otologic surgery.
The wide-angle view of the endoscope, along with its flexibility and ability to pivot, is particularly advantageous for removing lesions below the petrous apex and at the floor of the internal auditory canal. Furthermore, lesions surrounding the facial nerve can be approached without requiring nerve repositioning. The combined use of an endoscope and microscope, as a hybrid surgical approach, has emerged as an important technique in otologic microsurgery and minimally invasive lateral skull base surgery. Endoscopic ear surgery represents a significant leap forward in the development of otologic surgery, evolving from conventional otologic microsurgery. Like classic otologic microsurgery, modern endoscopic ear surgery is built upon foundational knowledge of microscopic anatomy of the ear and temporal bone, high-resolution imaging, and precise surgical techniques. It also demands a high level of technical skill and experience from surgeons.
Limitations of Endoscopic Ear Surgery
Endoscopic ear surgery faces certain challenges. Excessive bleeding can make surgical management difficult, and fogging of the endoscope lens can interfere with the operation. Additionally, the surgeon's need to hold the endoscope in one hand while performing the procedure with the other may hinder bimanual manipulation, making some intricate procedures more challenging and time-consuming, potentially leading to unnecessary tissue damage. These limitations can be mitigated by having an assistant hold the endoscope or suction device, using a fixed endoscope holder, or employing continuous irrigation techniques to maintain a clear field of view and improve surgical efficiency.
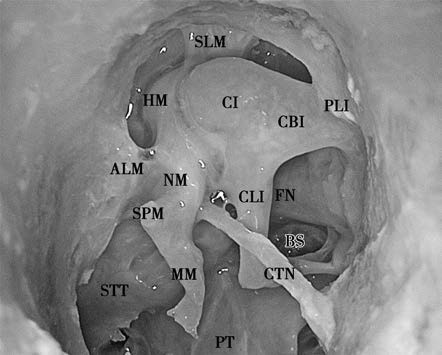
Figure 1 Illustration of the middle ear and ossicular structures of the left ear under an endoscope (the tympanic membrane has been removed).
HM: Head of the malleus
CI: Body of the incus
MM: Manubrium of the malleus
PT: Promontory
CBI: Short process of the incus
BS: Footplate of the stapes
CLI: Long process of the incus
SPM: Short process of the malleus
STT: Semicanal for the tensor tympani muscle
ALM: Anterior ligament of the malleus
NM: Neck of the malleus
SLM: Superior ligament of the malleus
FN: Tympanic segment of the facial nerve
PLI: Posterior ligament of the incus
CTN: Chorda tympani nerve
Indications and Contraindications for Endoscopic Ear Surgery
Indications
The most common indications include the removal of foreign bodies or neoplasms in the external auditory canal, myringotomy and tympanostomy tube placement, various types of tympanoplasty, ossiculoplasty, excision of tumors in the tympanic cavity, middle ear cholesteatoma removal, facial nerve decompression, eustachian tube balloon dilation, tenotomy of the stapedius and tensor tympani muscles, stapedectomy, and stapedial prosthesis implantation.
For middle ear diseases or lesions localized to the middle ear cavity and surrounding areas, endoscopic ear surgery offers significant technical advantages. This includes the ability to expose and remove hidden lesions, such as cholesteatomas, in complex areas like the facial recess, sinus tympani, anterior epitympanic recess, and eustachian tube region. Endoscopic-assisted lateral skull base surgeries, often combined with microscopic approaches, improve visualization and minimize invasiveness. Certain procedures involving the petrous apex are also feasible entirely under endoscopic guidance. High-resolution thin-slice CT scans of the temporal bone are crucial for preoperative planning, as they provide detailed images of ear anatomy and allow accurate assessment of the extent of tympanic cavity involvement. To differentiate the nature of lesions, enhanced MRI or non-echo planar imaging (non-EPI) diffusion-weighted imaging (DWI) MRI can be useful adjuncts.
Myringotomy and Tympanostomy Tube Placement
This is one of the best indications for endoscopic ear surgery and was among the first middle ear procedures performed endoscopically.
Tympanoplasty
Type I tympanoplasty (myringoplasty) is considered one of the most appropriate indications for endoscopic ear surgery. Whether using the overlay, underlay, or interlay techniques, the endoscope provides excellent operating space and visualization. Myringoplasty is also the most commonly performed middle ear surgery using an endoscope. The repair grafts typically include tragal cartilage, tragal cartilage-perichondrium composite grafts, or perichondrium. In Type II and III tympanoplasty, ossicular chain reconstruction and tympanic membrane repair are performed after the removal of pathological lesions, and the entire process can be completed under endoscopy. However, in cases with tympanosclerosis, particularly when widespread and rigid sclerotic plaques tightly encase the stapes, single-handed manipulation under endoscopy poses significant difficulties and risks, making the microscope a better option in these situations.
Ossiculoplasty
Endoscopy allows for detailed exploration of subtle abnormalities in the ossicular chain. Suitable ossicular prostheses, such as biocompatible implants or autologous ossicles, can be selected for ossicular chain reconstruction. Nevertheless, challenges arise during prosthesis placement due to single-handed manipulation under endoscopy and interference from blood or secretions; precise and successful completion requires advanced surgical skills and substantial experience.
Excision of Tumors in the Tympanic Cavity
Common examples include glomus tympanicum tumors. According to the Glasscock-Jackson classification, Type I and II tumors are confined primarily to the middle ear cavity and are suitable for endoscopic surgery. Techniques such as plasma ablation, bipolar suction coagulation, continuous irrigation, and the application of epinephrine-soaked sponges are often needed. Intraoperative considerations include avoiding tumor rupture and excessive bleeding to ensure clear visualization and complete excision. Type III and IV tumors, which involve the mastoid or extend further, are not suited for endoscopic surgery.
Middle Ear Cholesteatoma Removal
The more the middle ear is involved, the less feasible it becomes to preserve the ossicular chain. After removing ossicles, ossicular chain reconstruction using partial ossicular replacement prostheses (PORPs) or total ossicular replacement prostheses (TORPs) can be performed to minimize the air-bone gap.
Facial Nerve Decompression
Facial nerve decompression in the tympanic segment can be performed under endoscopic guidance. Achieving sufficient decompression often requires the temporary removal or excision of the incus to expose the affected area. Depending on the hearing status, ossiculoplasty may or may not be necessary following the decompression procedure.
Eustachian Tube Balloon Dilation
For eustachian tube dysfunction, balloon dilation may be performed via the tympanic orifice of the eustachian tube. However, in cases of simple balloon dilation alone, access through the nasopharynx or nasal cavity is preferable to avoid incisions. When eustachian tube dilation is performed along with other middle ear surgeries, access via the tympanic orifice in the ear canal is more straightforward. For patients with abnormal patency of the eustachian tube, narrowing procedures can also be performed endoscopically via the tympanic orifice.
Tenotomy of Tendons in the Tympanic Cavity
Procedures such as the tenotomy of the tensor tympani and stapedius tendons are easier to visualize and operate on under endoscopy compared to microscopy, with less disruption to normal structures.
Inner Ear Surgery
The most common procedure is stapedectomy, but endoscopy can also be used for localized inner ear tumors, semicircular canal fenestration or plugging, and as an adjunct in cochlear implantation surgery.
Lateral Skull Base Surgery
Procedures such as facial nerve vascular decompression and cerebellopontine angle tumor resection are typically performed with a combination of a microscope and endoscopic assistance.
Contraindications
Absolute contraindications include stenosis or atresia of the external auditory canal. Relative contraindications include extensive, firmly adhered, or highly vascularized lesions prone to significant bleeding.
Development and Outlook of Endoscopic Ear Surgery
Endoscopic ear surgery is known for its numerous advantages, such as its minimally invasive approach to directly access lesions and its ability to provide excellent exposure of deep, hidden, and complex areas. The process of its development represents the inevitable trajectory of any new technology, evolving from skepticism to acceptance and eventual standardization. The transformation brought about by endoscopic techniques has occurred within the framework of ear anatomy, physiology, and pathology. The fundamental principles and concepts guiding surgery under an endoscope remain consistent with those applied in surgery under a microscope.
As endoscopic technology continues to advance, accompanied by improvements in clinical diagnostic and therapeutic methods as well as innovations in surgical instrumentation, the integration of otologic microsurgery with endoscopic ear surgery is becoming even more seamless. By complementing each other, both techniques contribute to progress in surgeries involving the middle ear, inner ear, and lateral skull base, further advancing the field of otologic surgery.
Looking to the future, the empowerment of endoscopic ear surgery through artificial intelligence and surgical robotics is expected to drive even greater contributions in enhancing the diagnostic and therapeutic capabilities in otology.