Benign paroxysmal positional vertigo (BPPV) is a peripheral vestibular disorder characterized by recurrent episodes of brief vertigo and distinctive nystagmus triggered by changes in head position. It is often self-limiting, which is why it is referred to as "benign vertigo."
Epidemiology
BPPV is the most common peripheral vestibular disorder, accounting for about 20–40% of peripheral vertigo cases. The male-to-female ratio is approximately 1: (1.5–2), and it is more prevalent in individuals over the age of 40.
Etiology and Pathology
The etiology in approximately half of the cases is unknown, categorized as idiopathic BPPV. Idiopathic BPPV is more common in elderly individuals and in women, which may be related to accelerated degeneration of otoliths, reduced absorption capacity, and decreased otolith stability associated with aging. Hormonal changes, calcium metabolism disorders, and osteoporosis may also be predisposing factors. Secondary BPPV occurs as a result of other otological or systemic diseases. The most common causes include head trauma and vestibular neuritis. Other causes include Ménière’s disease, sudden hearing loss, infections or surgeries of the middle or inner ear, and prolonged bed rest. Surgical findings and histopathological studies of the temporal bone have revealed the presence of free-floating calcium carbonate crystals or basophilic deposits (otolith debris) in the semicircular canals or on the cupula of patients with BPPV.
Pathogenesis
The exact mechanism is unclear, but two widely recognized theories are the canalithiasis theory and the cupulolithiasis theory:
Canalithiasis
Otoconia that detach from the utricular macula accumulate in the endolymph of the long arm of the semicircular canal near the ampulla. During head movements, particularly when the head is placed in the provocative position, these otoconia move in the opposite direction of the ampulla. Their mass exerts a gravitational force, inducing endolymph flow that stimulates the ampullary crest, leading to nystagmus and vertigo.
Cupulolithiasis
Dislodged otoliths from the utricular macula adhere to the cupula on the ampullary side of the semicircular canal, increasing its sensitivity to gravitational changes and resulting in corresponding symptoms and signs.
Clinical Presentation
Symptoms
The hallmark symptom is the sudden onset of brief episodes of vertigo (typically lasting less than one minute) accompanied by nystagmus following changes in head position. The vertigo is often rotational in nature, though a minority of cases report a floating sensation. Patients may also experience nausea and vomiting as autonomic symptoms, but tinnitus, aural fullness, and hearing loss are absent. Vertigo and nystagmus resolve quickly upon maintaining a fixed head position, with each episode lasting a few seconds to a few tens of seconds, rarely exceeding one minute. Symptoms reoccur with subsequent changes in head position. Between attacks, patients may feel completely normal or may experience dizziness and mild imbalance. The disease course can range from several days to several months, with a few cases lasting years. It often resolves spontaneously but may recur, with variable intervals between episodes. Common triggering movements include getting in or out of bed, tilting the head forward, extending the head backward, turning over in bed, and rapid head turns.
BPPV is classified into four subtypes based on the affected semicircular canal: posterior canal BPPV, horizontal canal BPPV, anterior canal BPPV, and mixed-type BPPV. Posterior canal BPPV is the most common, accounting for approximately 90% of cases, followed by horizontal canal BPPV. Anterior canal BPPV is rare.
Examination
Positional Tests
Dix-Hallpike Test
This is a specific diagnostic test for posterior canal BPPV. The procedure involves positioning the patient on an examination table. The patient sits on the table with their head turned 45° to one side. With assistance, the patient is quickly moved into a supine position with the head hanging off the edge of the table at a 20° angle relative to the horizontal plane. Observations are made for 30 seconds or until nystagmus subsides before the patient is brought back to a sitting position. The other side is tested using the same method. In cases of posterior canal BPPV, positioning the affected ear downward triggers brief vertigo and nystagmus, while returning to the upright position may elicit similar responses. The nystagmus has the following characteristics:
- Vertical and rotational in direction.
- Starts with rapid intensification followed by gradual reduction.
- Displays a latency period, usually lasting a few seconds.
- Has a short duration, typically 5–10 seconds, and not exceeding one minute.
- Exhibits fatigue, with nystagmus diminishing or disappearing after repeated provocative positioning.
- Reverses direction when the head returns from the hanging position to the sitting position.
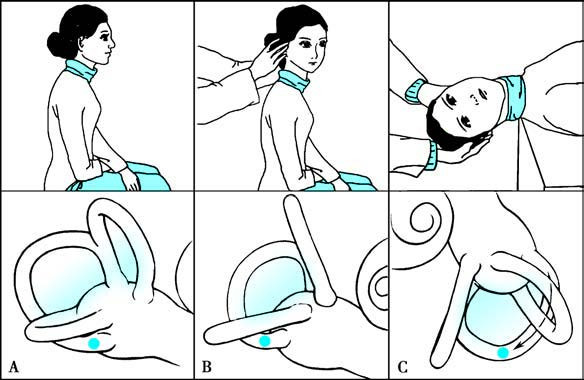
Figure 1 Schematic diagram of the Dix-Hallpike test
Roll Test
This is a specific diagnostic test for horizontal canal BPPV. The patient lies supine on the examination table and their head is quickly turned to the left or right side with assistance. Observations are made for up to one minute or until nystagmus stops. In cases of horizontal canal BPPV, rotational vertigo and horizontal nystagmus occur immediately (without latency). Geotropic nystagmus suggests canalithiasis and typically lasts 30–60 seconds, while apogeotropic nystagmus suggests cupulolithiasis and lasts longer than one minute.
Audiological Tests
Hearing remains generally normal.
Vestibular Function and Imaging Studies
These may assist in identifying the underlying cause or in differential diagnosis.
Diagnosis
Diagnostic Criteria:
- Recurrent and brief episodes of vertigo or dizziness (usually lasting no more than one minute) triggered by changes in head position relative to gravity.
- Positional tests elicit vertigo and characteristic positional nystagmus.
- Exclusion of other conditions, such as vestibular migraine, vestibular paroxysmia, central positional vertigo, Ménière’s disease, vestibular neuritis, labyrinthitis, superior semicircular canal dehiscence syndrome, posterior circulation ischemia, orthostatic hypotension, and psychogenic dizziness.
Differential Diagnosis
BPPV must be differentiated from central vertigo, Ménière’s disease, vestibular neuritis, superior semicircular canal dehiscence syndrome, and vertebrobasilar ischemia. Accurate determination of the affected semicircular canal should be made based on patient history and results of positional tests. Key points for distinguishing posterior canal BPPV from horizontal canal BPPV are provided in Table 1.
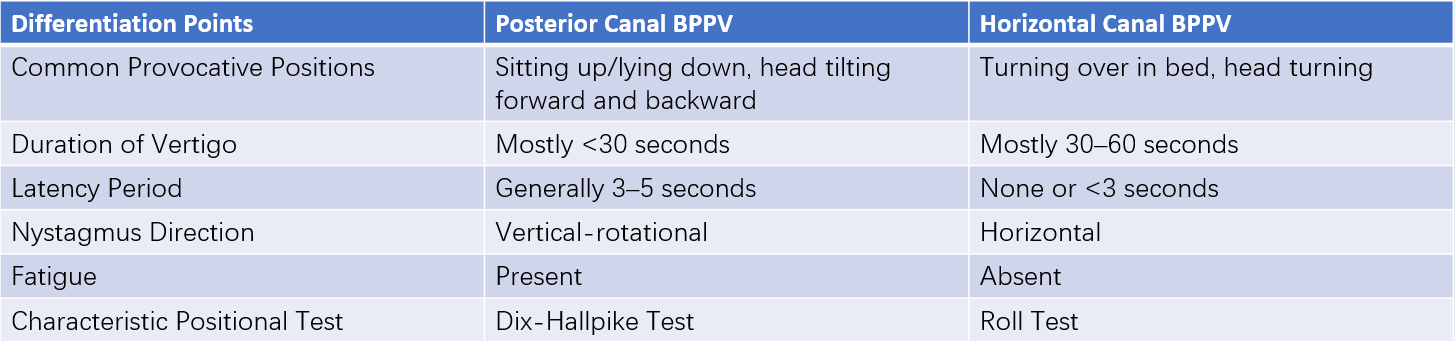
Table 1 Key points for differentiating posterior canal BPPV from horizontal canal BPPV
Treatment
BPPV generally has a self-limiting course, with the natural progression lasting from a few days to several months, rarely exceeding one year. Approximately 50% of cases resolve spontaneously within one month, but recurrence is possible. The most effective treatment method involves canalith repositioning procedures.
Canalith Repositioning Procedure (CRP)
Epley Maneuver
This is the most commonly used technique for treating posterior canal BPPV. It involves sequential changes in head position to facilitate the movement of otoliths out of the posterior canal under the influence of gravity. The patient sits on a treatment table with their head turned 45° towards the affected side. With assistance, the patient is quickly moved into a supine position with the head hanging off the edge of the table. The head is then rotated 90° to the unaffected side, corresponding to the unaffected side's Dix-Hallpike position. Next, the head and body are rotated together another 90° to the unaffected side so the patient is lying on their side with their face angled downwards at 135° from the supine position. The patient is then brought back to a sitting position, completing one maneuver cycle. Each position should be held for at least 30–60 seconds or until nystagmus subsides. The treatment process is repeated until no vertigo or nystagmus is observed in any position, followed by two to three additional cycles.
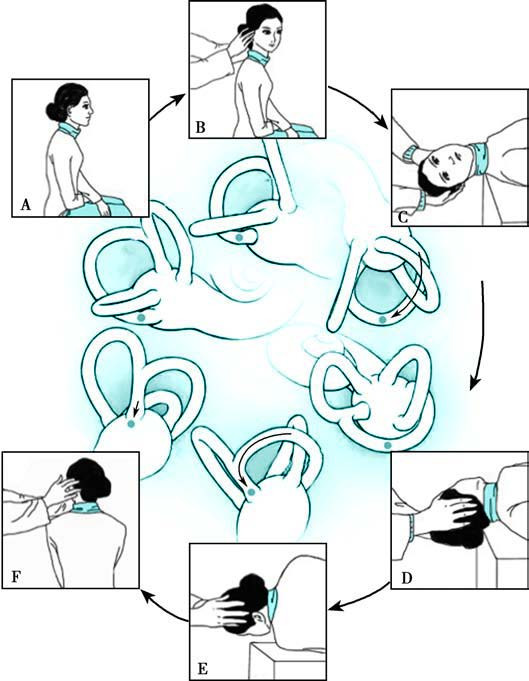
Figure 2 Schematic diagram of the Epley maneuver
Lempert Maneuver
Also known as the Barbecue Roll Maneuver, this is used to treat horizontal canal BPPV.
Otolith Repositioning Devices
These devices may be an alternative for patients where manual repositioning maneuvers are difficult to perform.
Medication Therapy
Medications generally do not reposition otoliths but may be used when other conditions coexist or when dizziness and balance issues persist after repositioning. Drugs that improve microcirculation in the inner ear, such as betahistine and ginkgo biloba extract, can be considered.
Surgical Treatment
For rare cases where manual repositioning fails to resolve symptoms and BPPV significantly interferes with daily life and work, semicircular canal occlusion surgery may be considered.
Vestibular Rehabilitation Training
Vestibular rehabilitation helps improve vestibular function through central adaptation and compensation mechanisms, alleviating residual symptoms caused by vestibular damage. It can serve as an adjunctive treatment alongside otolith repositioning in BPPV patients.