Atrioventricular (AV) block refers to a condition in which an abnormally prolonged refractory period in any part of the AV conduction system leads to delayed conduction or partial or complete failure of impulses to propagate from the atria to the ventricles. Clinically, AV block is classified into three degrees.
First-Degree Atrioventricular Block
First-degree AV block is characterized by prolonged AV conduction time. On electrocardiograms, the PR interval exceeds the normal range, but every atrial impulse is conducted to the ventricles.
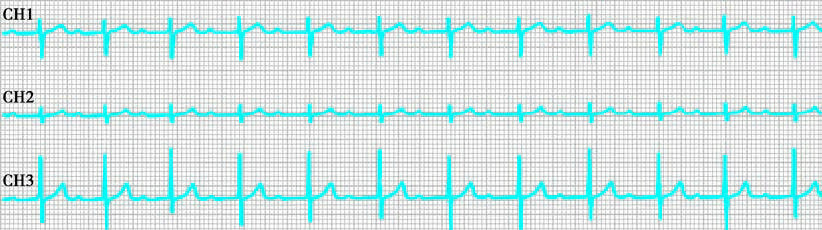
Figure 1 Electrocardiographic features of first-degree atrioventricular block
Second-Degree Atrioventricular Block
In second-degree AV block, not all impulses from the sinoatrial node are conducted to the ventricles, leading to missed beats of varying degrees. It is further divided into two types:
Mobitz Type I (Wenckebach Phenomenon)
This type is characterized by progressive prolongation of the PR interval until a P wave is not followed by a QRS complex. The RR interval typically shortens progressively, and the distance between the two R waves bracketing the dropped beat is less than twice the shortest RR interval.
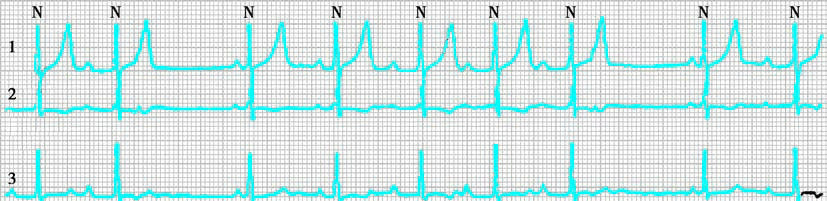
Figure 2 Electrocardiographic features of second-degree atrioventricular block (Mobitz Type I)
Mobitz Type II
This type is characterized by a fixed PR interval, with some atrial impulses failing to conduct to the ventricles. Intermittent ventricular misses occur, often accompanied by QRS complex widening.
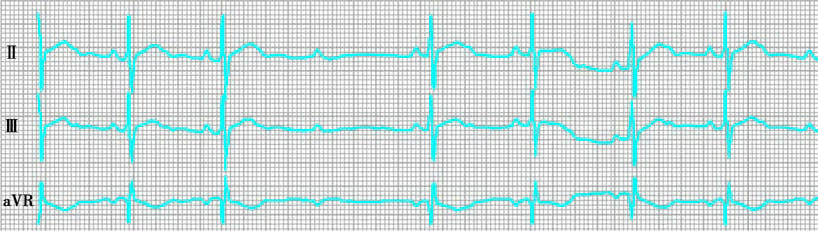
Figure 3 Electrocardiographic features of second-degree atrioventricular block (Mobitz Type II)
Third-Degree Atrioventricular Block
In third-degree AV block, the effective refractory period is so extensively prolonged that all P waves fall within the refractory period and fail to propagate to the ventricles. The atria and ventricles function independently of each other. The ventricular rate is slower than the atrial rate.

Figure 4 Electrocardiographic features of third-degree atrioventricular block
Etiology
First-degree AV block may occasionally be observed in normal, healthy children but can also occur due to rheumatic carditis, viral myocarditis, fever, nephritis, or congenital heart disease. The use of digitalis can also prolong the PR interval.
Second-degree AV block may result from rheumatic heart disease, myocarditis caused by various etiologies, severe hypoxia, post-cardiac surgery, or congenital heart diseases (especially transposition of the great arteries).
Third-degree AV block, also called complete AV block, is rare in children. Its etiology can be congenital or acquired. In congenital cases, approximately 50% of affected children have no structural cardiac abnormalities, while others may present with congenital heart diseases or endocardial fibroelastosis. Acquired causes are most commonly related to cardiac surgery, followed by viral myocarditis. Neonatal hypocalcemia and acidosis may lead to temporary cases of third-degree AV block.
Clinical Manifestations
First-degree AV block generally has no adverse hemodynamic effects. Clinical examination may only reveal a muffled first heart sound, with no other specific findings. Diagnosis primarily relies on electrocardiographic findings.
The clinical presentation of second-degree AV block depends on the underlying cardiac pathology and the hemodynamic changes caused by the conduction disorder. Bradycardia may result in chest tightness, palpitations, dizziness, or syncope. Auscultation may reveal irregular rhythm and missed beats, apart from the changes associated with the primary heart disease. Mobitz Type I is more common than Type II, although Type II has a poorer prognosis and is more likely to progress to complete AV block, leading to Stokes-Adams syndrome.
In third-degree AV block, some children may remain asymptomatic, while others present with fatigue, dizziness, or shortness of breath during physical activity due to reduced cardiac output. Severe cases may exhibit Stokes-Adams syndrome, characterized by loss of consciousness or even sudden death. Some children may also have symptoms of heart failure or reduced tolerance to stress. Physical examination typically reveals a slow and regular pulse, with variable intensity of the first heart sound. Third or fourth heart sounds may sometimes be audible. A soft systolic ejection murmur (grade 1/6 to 2/6) at the base of the heart may be observed in most cases due to relative semilunar valve stenosis caused by the increased stroke volume. Mid-diastolic murmurs may also be present due to increased blood flow across the AV valves. Chest X-rays may show evidence of cardiomegaly in 60% of uncomplicated cases of third-degree AV block.
Treatment
Treatment of first-degree AV block typically focuses on addressing the underlying cause, with no specific intervention usually necessary.
For second-degree AV block, management should target the primary condition. Treatment, including atropine or isoproterenol, may be used to address severe bradycardia or reduced cardiac output.
Third-degree AV block with symptoms of heart failure or features of Stokes-Adams syndrome requires more aggressive treatment. Correction of hypoxia and acidosis may improve cardiac conduction function. Corticosteroids can reduce localized edema in cases caused by myocarditis or transient surgical injury. Oral atropine, ephedrine, or sublingual isoproterenol may be effective. Severe cases may require subcutaneous or intravenous atropine. Pacemaker implantation is indicated for recurrent Stokes-Adams syndrome, failure of medication, or concurrent heart failure. Temporary pacing should precede permanent pacemaker placement if normal conduction recovery is expected. Permanent pacing may be considered if recovery does not occur within approximately four weeks.
Prognosis
The prognosis for first-degree AV block is generally favorable. The prognosis of second-degree AV block depends on the underlying cardiac condition. Third-degree AV block prognosis is influenced by associated cardiac abnormalities and the severity of the disease. The use of pacemakers significantly improves outcomes in affected individuals.