Ventricular tachycardia (VT) refers to a tachycardia originating below the bifurcation of the bundle of His, characterized by three to five or more wide and abnormal QRS complexes.
Etiology
The condition may result from cardiac surgery, cardiac catheterization, severe myocarditis, congenital heart disease, infection, hypoxia, or electrolyte disturbances. However, the etiology remains unclear in many cases.
Clinical Manifestations
The clinical presentation is similar to paroxysmal supraventricular tachycardia but tends to be more severe. Children often exhibit restlessness, pallor, and rapid breathing, while older children may report palpitations or precordial pain. Severe cases may involve syncope, shock, and congestive heart failure. Hemodynamic changes are generally mild in short episodes but may become significant if episodes persist for more than 24 hours. Physical examination may reveal an increased heart rate, often exceeding 150 beats per minute, with a regular rhythm and heart sounds of varying intensity.
Diagnosis
Electrocardiographic features include:
- Ventricular rates typically ranging from 150 to 250 beats per minute, with wide and abnormal QRS complexes and prolonged duration.
- T wave polarity opposite to the main deflection of the QRS complex, and a lack of a fixed relationship between P waves and QRS complexes.
- The QT interval is often normal but may show prolongation, especially in cases of polymorphic VT.
- Atrial rates are slower than ventricular rates, and ventricular fusion beats or ventricular capture may occasionally be observed.
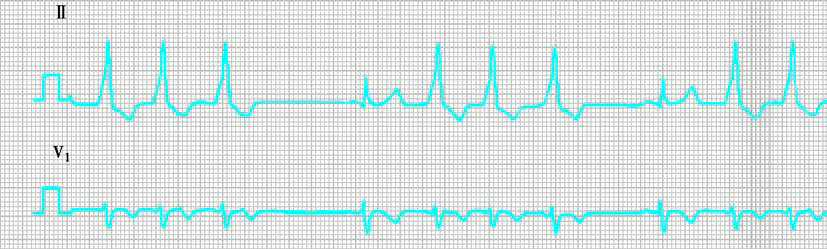
Figure 1 Electrocardiographic features of ventricular tachycardia
Electrocardiography serves as a key diagnostic tool for VT. However, distinguishing VT from supraventricular tachycardia with aberrant ventricular conduction can sometimes be challenging, requiring careful assessment of clinical history, physical examination findings, ECG characteristics, and the response to treatment interventions.
Treatment
Lidocaine is a commonly used medication for controlling VT, though its effects are short-lived. Excessive doses may cause toxic reactions such as seizures or conduction block. For patients experiencing blood pressure decline or heart failure, synchronized direct current cardioversion is the first-line treatment, with lidocaine used thereafter for maintenance. Propafenone, amiodarone, or sotalol may be administered orally to prevent recurrence.
In cases of polymorphic VT with QT interval prolongation, treatment depends on the underlying cause. For congenital factors, beta-blockers are the first choice, while class Ia, Ic, and III antiarrhythmic drugs, as well as isoproterenol, are contraindicated. For acquired causes, isoproterenol may be considered, with lidocaine as an alternative if necessary.
Prognosis
VT is a serious form of tachyarrhythmia that carries a risk of progression to ventricular fibrillation and sudden death. In cases with underlying heart disease, the mortality rate can exceed 50%, highlighting the importance of timely diagnosis and appropriate management.