Premature beat (also known as premature contraction or premature depolarization) refers to impulses originating from ectopic foci in the heart, making it the most common arrhythmia in pediatric populations. Ectopic pacemaker sites can be located in the atria, atrioventricular (AV) junction, or ventricular tissues, resulting in atrial, junctional, and ventricular premature beats, respectively. Among these, ventricular premature beats are the most frequently observed.
Etiology
Premature beats commonly occur in children without underlying organic heart disease. They may be triggered by fatigue, emotional stress, or autonomic nervous system instability. However, they can also be associated with conditions such as myocarditis, congenital heart disease, or rheumatic heart disease. Other causes include drug toxicity (e.g., sympathomimetic agents, digitalis, quinidine), hypoxia, acid-base imbalance, electrolyte disturbances (e.g., hypokalemia), cardiac catheterization, and heart surgery. Approximately 1–2% of healthy school-aged children experience premature beats.
Clinical Manifestations
Symptoms in children are typically milder than in adults, and subjective complaints are often absent. Some older children may report palpitations, chest tightness, or discomfort. The frequency of premature beats varies among individuals and can show significant fluctuations over time in the same patient. In some children, premature beats may decrease during exercise-induced tachycardia, while in others, the frequency may increase, which could indicate the presence of underlying organic heart disease. Electrocardiographic (ECG) evaluation is essential for accurate diagnosis, determination of premature beat type, and characterization of features based on the presence of P′ waves, P′ wave morphology, PR interval duration, and QRS wave morphology.
Diagnosis
ECG Features of Atrial Premature Beats
These include:
- Premature P′ waves, which may overlap with the preceding T wave.
- PR intervals are within the normal range.
- Incomplete compensatory pauses following premature beats.
- Abnormal QRS morphology, if present, is due to intraventricular conduction disturbances.
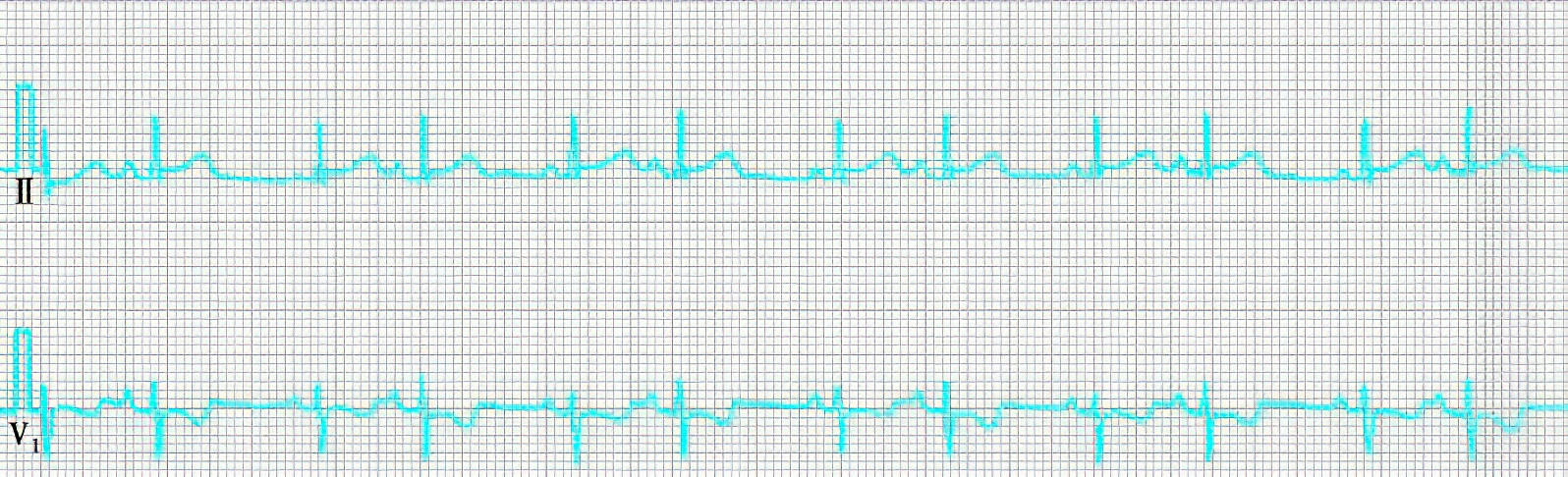
Figure 1 Electrocardiographic features of atrial premature beats
ECG Features of Junctional Premature Beats
These include:
- Premature QRS waves with morphology and duration that resemble normal sinus QRS complexes.
- Retrograde P′ waves appearing before or after the QRS complex, with P′R interval <0.10 seconds. These P′ waves may sometimes overlap with QRS complexes, making them difficult to identify.
- Compensatory pauses are often incomplete.

Figure 2 Electrocardiographic features of junctional premature beats
ECG Features of Ventricular Premature Beats
These include:
- Premature QRS waves without preceding ectopic P waves.
- Widened and abnormal QRS complexes with T waves oriented opposite to the main QRS deflection.
- Complete compensatory pauses following the premature beats.

Figure 3 Electrocardiographic features of ventricular premature beats
Treatment
Antiarrhythmic treatment is warranted for premature beats occurring in the context of organic heart disease, for patients with noticeable symptoms, or for those with multiform premature beats on ECG. Treatment should be based on the type of premature beat. Medications such as propafenone or propranolol can be administered. If atrial premature beats do not respond to these drugs, digitalis preparations may be considered. For ventricular premature beats, drugs like lidocaine, mexiletine, or moricizine may be used in necessary cases. Additionally, any underlying disease should be treated with targeted therapy.
Prognosis
Pharmacological treatment yields good outcomes. For patients with infrequent premature beats, no subjective symptoms, or frequent but monomorphic premature beats with decreases or resolution during physical activity, treatment may not be necessary. In some individuals, premature beats may persist for years, but many cases eventually resolve spontaneously.