Medical History and Physical Examination
Medical History Inquiry
Common symptoms of cardiovascular diseases in children include feeding difficulties, reduced exercise tolerance, rapid breathing, dyspnea, cyanosis, delayed growth and development, and hypoxic spells. Other symptoms may include edema, syncope, palpitations, and chest pain. Congenital heart disease is the most common cardiovascular condition in children under three years old. Evidence for significant left-to-right shunting includes recurrent pneumonia, heart failure, and delayed growth and development. Infantile heart failure primarily manifests as shallow and rapid breathing, feeding difficulties, and excessive sweating. Hoarseness may occur if an enlarged left atrium or pulmonary artery compresses the recurrent laryngeal nerve. For cases with cyanosis, it is essential to consider and rule out respiratory system diseases and inquire about signs such as squatting and hypoxic spells.
Rheumatic heart disease is more common in older children, where it is important to look for a history of sore throat, migratory joint pain, or chorea. In cases involving chest discomfort, palpitations, or precordial pain, arrhythmias and myocardial diseases should be considered. Kawasaki disease has become a leading cause of acquired heart disease in children in developed regions. It primarily affects the coronary arteries and is most common in children under five years old. Distinctive clinical manifestations include symptoms involving the skin, mucous membranes, and lymph nodes.
The medical history should also include whether the mother had viral infections, radiation exposure, harmful substance exposure, or drug use during early pregnancy, as well as any family history of hereditary diseases. Many congenital heart defects and cardiomyopathies have genetic associations.
Physical Examination
General Examination
Assessment of physical growth and development is important, including observation of specific facial features, systemic congenital anomalies, mental state, body position, and respiratory rate. Examination should include checking for cyanosis in areas with rich capillary networks, such as the lips, nasal tip, and fingertips/toe tips, and for the presence of clubbing. Petechiae on the skin and mucous membranes are suggestive of embolic phenomena in infective endocarditis, while subcutaneous nodules and erythema marginatum are key manifestations of rheumatic fever. Observation of jugular vein pulsations, hepatojugular reflux, liver and spleen size and tenderness, as well as the presence of edema in the lower extremities, is also necessary.
Cardiac Examination
Inspection
The presence of precordial bulging, the location, intensity, and range of the apical impulse should be noted. Precordial bulging often indicates cardiomegaly and should be distinguished from pectus carinatum caused by rickets. In normal children under two years of age, the apical impulse is located in the 4th intercostal space on the left side, extending up to 1 cm beyond the midclavicular line; by 5–6 years of age, it shifts to the 5th intercostal space along the midclavicular line. The normal range of the apical impulse is within 2–3 cm2. A forceful and enlarged apical impulse indicates ventricular hypertrophy. Left ventricular hypertrophy typically shifts the point of maximal impulse downward and to the left, while right ventricular hypertrophy causes a diffuse, sometimes subxiphoid apical impulse. A weakened apical impulse may indicate pericardial effusion or reduced myocardial contractility. In cases of dextrocardia, the apical impulse is observed on the right side. The apical impulse is more visible in thin children and less visible in obese children.
Palpation
The position, intensity, and range of the apical impulse should be further confirmed, along with any precordial lifting or thrills. Lifting in the 5th or 6th intercostal space lateral to the midclavicular line suggests left ventricular hypertrophy, while lifting along the left sternal border in the 3rd or 4th intercostal spaces or in the subxiphoid region suggests right ventricular hypertrophy. The location of thrills aids in identifying the source of murmurs.
Percussion
A rough estimate of the heart's position and size can be made.
Auscultation
Attention should be paid to heart rate, rhythm, the intensity of the first and second heart sounds, whether they are accentuated, diminished, or absent, and whether there are any splits, particularly the significance of the second heart sound (P2) in the pulmonary valve area. An accentuated P2 suggests pulmonary hypertension, while a diminished P2 supports the diagnosis of pulmonary stenosis. In normal children, physiological splitting of P2 may occur during inspiration, while fixed splitting of P2 is a key sign of atrial septal defect. Murmurs are crucial in diagnosing congenital heart defects, requiring evaluation of their location, quality, intensity, timing, and radiation.
Peripheral Vascular Signs
Peripheral vascular assessment should include comparison of the pulse and blood pressure in the four extremities. Diminished or absent femoral pulses and lower limb blood pressure lower than upper limb blood pressure suggest coarctation of the aorta. Widened pulse pressure, along with capillary pulsations and a "gunshot" femoral pulse, indicates conditions such as patent ductus arteriosus or aortic regurgitation.
Auxiliary Examinations
Measurement of Peripheral Pulse Oximetry
Hypoxemia is common in many complex congenital heart diseases, especially in critically ill neonates who may exhibit hypoxemia during the neonatal period. Cyanosis becomes evident when arterial oxygen saturation drops below 80%. However, cyanosis may not be visually apparent when oxygen saturation is between 80% and 95%. Therefore, pulse oximetry (POX) is commonly used in clinical practice to identify hypoxemia. POX is highly favored for its non-invasive nature and accuracy. It is a simple method; in children, finger clip or electrode devices can be placed on the fingertip or earlobe for detection, while specialized wrap-around electrodes are used for neonates, placed circumferentially around the right palm and one foot for oxygen saturation measurement. Data is recorded once the heart rate displayed by the pulse oximeter matches the actual heart rate of the neonate, and the oxygen saturation value and waveform are stable for at least 10 seconds. An oxygen saturation consistently below 95% or a difference greater than 3% between the upper and lower extremities is considered abnormal.
Early screening for critical congenital heart disease is performed through a combination of POX and auscultation for heart murmurs. However, POX results can sometimes be affected by factors such as peripheral vascular filling, skin pigmentation, limb movement, or poor contact between the probe and the limb.
Standard X-ray Examination
This includes chest fluoroscopy and radiography. Fluoroscopy can dynamically observe the pulsation, position, and morphology of the heart and great vessels, as well as the caliber and distribution of pulmonary vessels; however, it cannot detect fine structural abnormalities. Radiographic imaging compensates for this limitation, provides permanent records, and commonly includes standard posterior-anterior (PA) and lateral views, with oblique views as necessary. The following aspects are important when analyzing chest X-rays:
Quality of Radiographs
Ideal chest radiographs should be taken during inspiration, with clear visualization of lung markings, good contrast, and sharp outlines of the cardiac silhouette. The thoracic spine and intervertebral spaces behind the heart should also be visible.
Determination of Cardiac Position and Assessment of Situs Abnormalities
The positions of the liver, gastric bubble, and diaphragm are critical. High-voltage chest radiographs (100–140kV) may be used to observe bronchial anatomy.
Cardiothoracic Ratio
In older children, the cardiothoracic ratio should be less than 50%; in infants and young children, it should be less than 55%. The ratio increases during expiration or when the patient is in a supine position.
Pulmonary Vasculature
Examination of pulmonary vasculature assesses whether it is congested or underperfused, and whether collateral vessels have formed.
Cardiac Morphology and Structural Abnormalities
Evaluation includes the shape, position, and enlargement of cardiac chambers, the displacement of vessels, whether the pulmonary artery segment is prominent or recessed, and whether the aortic arch is dilated or narrowed.
Electrocardiogram (ECG)
The ECG is highly specific for detecting arrhythmias and provides meaningful insights regarding atrial and ventricular hypertrophy, conduction block, electrolyte imbalances, and drug toxicity. It is also a valuable reference for determining cardiac position and myocardial abnormalities. Additional information can be gained through 24-hour Holter monitoring and stress ECG tests.
When analyzing pediatric ECGs, the following age-related considerations are important:
- Younger children have faster heart rates, shorter intervals, and narrower wave durations. Some normal values differ from those in adults.
- The QRS complex is dominated by the right ventricle in neonates and infants, gradually transitioning to left ventricular dominance with age.
- The T wave in the right precordial leads changes with age. For instance, on the first day after birth, the T wave in lead V1 is upright, but by 4–5 days, it inverts or becomes biphasic.
Echocardiography
Echocardiography provides detailed anatomical information, functional assessment, and hemodynamic data, enabling accurate diagnosis of most congenital heart diseases. It has largely replaced invasive cardiac catheterization and angiography.
Transthoracic echocardiography is the standard method, but transesophageal echocardiography (TEE) is also widely used. TEE involves placing the ultrasound probe in the esophagus or gastric fundus and is primarily used for intraoperative monitoring and assessment of surgical outcomes. The following echocardiographic techniques are commonly employed:
M-mode Echocardiography
M-mode echocardiography records motion curves of cardiac structures based on ultrasound reflections. It is particularly useful for assessing valve motion, measuring cardiac chambers and vessel diameters, and calculating functional parameters such as left ventricular ejection fraction and fractional shortening in conjunction with simultaneously recorded ECGs.
Two-dimensional Echocardiography
Two-dimensional imaging provides real-time sectional views of cardiac and great vessel anatomy, their movements, and spatial relationships. It forms the foundation of echocardiographic assessments.
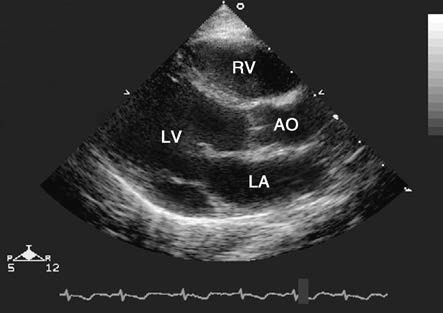
Figure 1 Long-axis view of the left heart on a two-dimensional echocardiogram
LA—Left Atrium; LV—Left Ventricle; AO—Aorta; RV—Right Ventricle.
The image shows mitral valve opening and aortic valve closure during diastole.
Doppler Echocardiography
Doppler techniques, including spectral Doppler (pulsed and continuous wave) and color flow imaging, assess blood flow direction and velocity. Pressure gradients are calculated to evaluate valve or vascular stenosis, estimate shunt volumes of intracardiac defects, assess pulmonary artery pressure, and evaluate cardiac function.
Three-dimensional Echocardiography
Three-dimensional imaging offers intuitive and vivid spatial views, enabling better recognition of cardiac structures. It allows arbitrary sectioning of images to fully display areas of interest, providing surgical simulations and detailed guides for selecting incision sites.
Cardiac Catheterization
Cardiac catheterization is an important method for further confirming the diagnosis of congenital heart disease and making preoperative decisions. Based on the site of evaluation, it can be classified into right heart catheterization and left heart catheterization. Right heart catheterization involves percutaneous puncture of the femoral vein, advancing a radiopaque catheter through the inferior vena cava, right atrium, and right ventricle, and into the pulmonary artery. Left heart catheterization involves advancing the catheter retrogradely through the femoral artery and descending aorta to the left ventricle. During the procedure, anomalous pathways are investigated, and measurements of oxygen saturation and pressure are obtained from different locations within the heart chambers and major vessels. Cardiac output, shunt volumes, and vascular resistance can be calculated. Measurement of pulmonary capillary wedge pressure provides insights into the state of the pulmonary vascular bed in patients with pulmonary hypertension and holds clinical significance for identifying inflow and outflow tract abnormalities of the left atrium and assessing left ventricular function. Continuous pressure measurements help in evaluating the location, type, and severity of valve or vascular stenosis. In addition, cardiac catheterization can also allow for endomyocardial biopsy and electrophysiological assessments.
Cardiovascular Angiography
During cardiac catheterization, the catheter tip is guided to the targeted heart chamber or vascular region based on diagnostic needs. Angiography is performed from axial or angled projections according to specific requirements for visualizing pathological changes in different locations. Rapid imaging or cineangiography is used to clarify anatomical abnormalities in the cardiovascular system. Despite advancements in non-invasive techniques, this remains a crucial method for evaluating complex congenital cardiovascular anomalies. The development of digital subtraction angiography (DSA) technology, along with the use of next-generation contrast agents, has improved diagnostic precision while minimizing harm to the body during angiography.
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging offers advantages such as the absence of ionizing radiation and the capability for multi-planar imaging. Various techniques, including spin-echo (SE), cine-MRI, magnetic resonance angiography (MRA), and three-dimensional MRI, are available for different diagnostic purposes. MRI is commonly used for identifying abnormalities in large extracardiac vessels, such as aortic arch malformations.
Computed Tomography (CT)
Electron beam computed tomography (EBCT) and spiral CT are now applied in the cardiovascular field. These methods provide high diagnostic value for conditions such as abnormalities of large extracardiac vessels and their branches, calcification of cardiac valves, pericardium, and vascular walls, intracardiac masses, pericardial constriction, and cardiomyopathies. Additionally, CT can effectively demonstrate airway narrowing caused by vascular rings compressing the trachea or bronchi.
Radionuclide Cardiac Imaging
Radionuclide imaging is primarily utilized for evaluating cardiac function, quantifying left-to-right shunting, and assessing myocardial ischemia. A commonly used radionuclide is technetium-99m (99mTc), which is administered intravenously. A gamma scintillation camera detects the gamma rays emitted by the radionuclide, converting them into pixel pulses. All data are recorded and stored by a computer, followed by image reconstruction and analysis.