Acute infectious laryngitis refers to an acute diffuse inflammation of the mucosa of the larynx. Clinically, it is characterized by barking cough, hoarseness, stridor, and inspiratory dyspnea. In some cases, the trachea and bronchi may also be involved, leading to acute laryngotracheobronchitis. It is more common in infants and young children, with a higher incidence during the winter and spring seasons.
Etiology
The condition is caused by viral or bacterial infections and may also occur as a complication of acute infectious diseases such as measles, pertussis, and influenza. Common viruses include parainfluenza virus, influenza virus, and adenovirus, while common bacteria include Staphylococcus aureus, Streptococcus spp., and Streptococcus pneumoniae. Due to the anatomical characteristics of the larynx in children, inflammation often leads to congestion and edema, increasing the risk of laryngeal obstruction.
Clinical Manifestations
The onset is acute, and the symptoms are severe. Clinical features may include fever, barking cough, hoarseness, inspiratory stridor, and retractions during inspiration. Severe cases may present with cyanosis, restlessness, pallor, and an increased heart rate. Examination of the throat often reveals congestion, and indirect laryngoscopy may show varying degrees of congestion and edema in the larynx and on the vocal cords. Symptoms are generally milder during the daytime but tend to worsen at night after sleep. If laryngeal obstruction is not relieved in time, asphyxia and death may occur. The severity of inspiratory dyspnea is used to classify laryngeal obstruction into four grades.
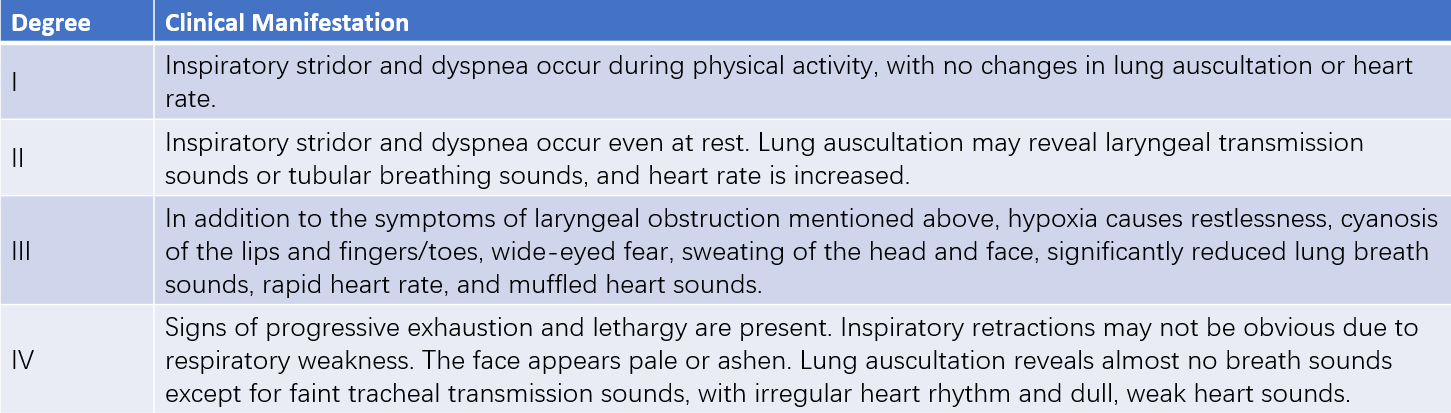
Table 1 Degrees of laryngeal obstruction
Diagnosis and Differential Diagnosis
Diagnosis is usually straightforward based on the clinical features of acute onset, barking cough, hoarseness, stridor, and inspiratory dyspnea. However, it is important to differentiate this condition from other causes of laryngeal obstruction, such as diphtheria, acute epiglottitis, laryngospasm, foreign bodies in the larynx or trachea, and congenital anomalies of the larynx.
Treatment
General Treatment
Ensuring adequate rest and hydration while maintaining airway patency to prevent worsening hypoxia is important.
Glucocorticoids
Glucocorticoids have anti-inflammatory, antiallergic, and immunosuppressive properties. Their use can help reduce laryngeal edema and alleviate laryngeal obstruction. Glucocorticoid therapy is recommended for children with grade II or higher laryngeal obstruction. Commonly used medications include prednisolone, prednisone, dexamethasone, and hydrocortisone. Nebulized glucocorticoid therapy (e.g., budesonide suspension) may also provide some benefit.
Infection Control
Most cases are caused by viral infections. If bacterial infection is suspected, appropriate and adequate broad-spectrum antibiotic therapy may be initiated promptly.
Symptomatic Treatment
Oxygen therapy is beneficial for children experiencing hypoxia. Although sedatives may reduce restlessness, their use can mask symptoms of hypoxia and suppress respiratory effort, and should typically be avoided. Expectorants may be used for patients with excessive mucus production.
Endotracheal Intubation
For children showing signs of severe hypoxia despite other interventions or with grade III or higher laryngeal obstruction, prompt endotracheal intubation and mechanical ventilation support may be necessary. Tracheotomy may be considered in extreme cases.