Important Signs During Physical Examination of the Respiratory System
Changes in Respiratory Rate
An increase in respiratory rate is considered an early sign of respiratory distress, and this is more pronounced in younger children. Tachypnea is diagnosed when the respiratory rate meets or exceeds the following thresholds:
- <2 months of age: ≥60 breaths/min
- 2–12 months: ≥50 breaths/min
- 1–5 years: ≥40 breaths/min
- 5 years: ≥30 breaths/min
A decrease in respiratory rate or irregular breathing rhythm is also considered a dangerous sign.
Retraction during Inspiration
Indrawing at the suprasternal notch, supraclavicular fossa, intercostal spaces, or subxiphoid area during inspiration may occur in cases of upper airway obstruction or severe pulmonary disease.
Specific Breathing Patterns
Inspiratory Stridor
The normal ratio of inspiratory time to expiratory time (I:E) in children is 1:(1.5–2.0). The presence of stridor during inspiration, accompanied by prolonged inspiratory time, indicates upper airway obstruction.
Expiratory Grunting
This is a sign of lower airway obstruction and poor lung expansion, particularly common in infantile respiratory distress syndrome.
Abnormal Breath Sounds
Wheezing
Wheezing is more prominent during expiration and suggests obstruction of small bronchi. In cases of severe small airway obstruction, wheezing may be absent, and diminished or absent breath sounds may be heard instead. This condition, referred to as "silent lung," is commonly seen in severe asthma and is an indication of critical illness.
Crackles
Inconsistent medium- to coarse crackles are often caused by secretions in the bronchi. Fine crackles heard during the inspiratory phase, especially at the end of deep inspiration, are typically associated with alveolar secretions and are commonly seen in conditions such as pneumonia. In infants with shallow and rapid breathing, crackles may not always be obvious; they may become detectable after triggering crying to induce deep breaths near the end of inspiration.
Cyanosis
Cyanosis is a key manifestation of reduced blood oxygenation.
- Peripheral Cyanosis: Caused by slow blood flow and a larger arteriovenous oxygen difference in regions such as the extremities.
- Central Cyanosis: Occurs in areas with faster blood flow and a smaller arteriovenous oxygen difference, such as the tongue and mucosa. Central cyanosis develops later than peripheral cyanosis but is of greater clinical significance.
Clubbing of Fingers/Toes
Clubbing results from chronic hypoxia and is characterized by dorsal soft tissue proliferation at the distal phalanges, causing elevation of the nail bed. It can be observed in children with conditions such as bronchiectasis and chronic pneumonia.
Examination Methods
Blood Gas Analysis
Blood gas analysis reflects gas exchange and the acid-base balance of blood and provides a basis for diagnosis and treatment. Under conditions of sea level, one atmospheric pressure, and resting state in ambient air, respiratory failure is diagnosed when:
- Arterial oxygen pressure (PaO2) <60 mmHg (8.0 kPa)
- Arterial carbon dioxide pressure (PaCO2) >50 mmHg (6.67 kPa)
- Arterial oxygen saturation (SaO2) <85%.
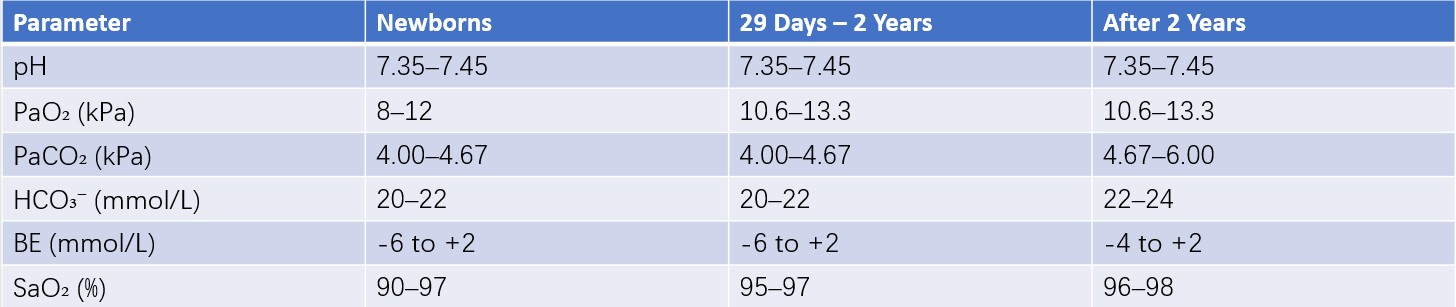
Table 1 Reference values for pediatric blood gas analysis
Note: 1 kPa = 7.501 mmHg.
Chest Imaging
Chest X-rays remain the foundational imaging tool for diagnosing respiratory diseases. Diagnostic capabilities for pediatric respiratory diseases have been greatly enhanced by advances in computed tomography (CT), particularly high-resolution CT (HRCT), and magnetic resonance imaging (MRI). Digital chest X-ray imaging can quickly generate and relay clear radiographic images of the lungs.
High-Resolution CT (HRCT)
HRCT is valuable for diagnosing many lung diseases and can reveal key features suggestive of interstitial lung diseases, such as ground-glass opacities, reticular patterns, and consolidation. It can also show thickening of interlobular septa. Three-dimensional reconstruction clearly delineates the internal and external structures of the trachea and bronchi.
MRI
MRI is superior to CT in determining the relationship between masses and pulmonary hilum or mediastinal vessels. It is particularly suitable for evaluating hilar or mediastinal tumors or metastatic lymph nodes. Using three-dimensional imaging techniques, it can detect intravascular thrombi in segmental pulmonary lobes.
Bronchoscopy in Children
Fiberoptic bronchoscopy, electronic bronchoscopy, and hybrid bronchoscopy are suitable for diagnosing and differentiating the causes of respiratory tract disorders such as unexplained hemoptysis, chronic or recurrent cough and wheezing, and atelectasis. These techniques are also valuable in identifying the etiology and pathogens of severe or refractory pneumonia. Bronchoscopy can improve airway patency through procedures like foreign body removal and bronchial lavage. In recent years, interventional bronchoscopic techniques, such as balloon dilation, stent placement, cryotherapy, and laser treatment, have been applied in pediatric clinical practice, significantly enhancing the diagnostic and therapeutic capabilities for complex respiratory diseases.
Pulmonary Function Testing
Pulmonary function testing, which measures and evaluates respiratory function using specialized methods and instruments, represents an important approach to assessing lung performance. A more comprehensive pulmonary function assessment can be performed on children over the age of 5 years. Impulse oscillometry system (IOS) technology requires relatively low levels of patient cooperation, allowing most preschool-aged children to complete the test. For children over the age of 3 years, IOS testing is feasible. For children under 3 years of age, pulmonary function testing can involve methods such as tidal breathing flow-volume (TBFV) curve analysis, partial forced expiratory techniques, occlusion methods, or even infant plethysmography.
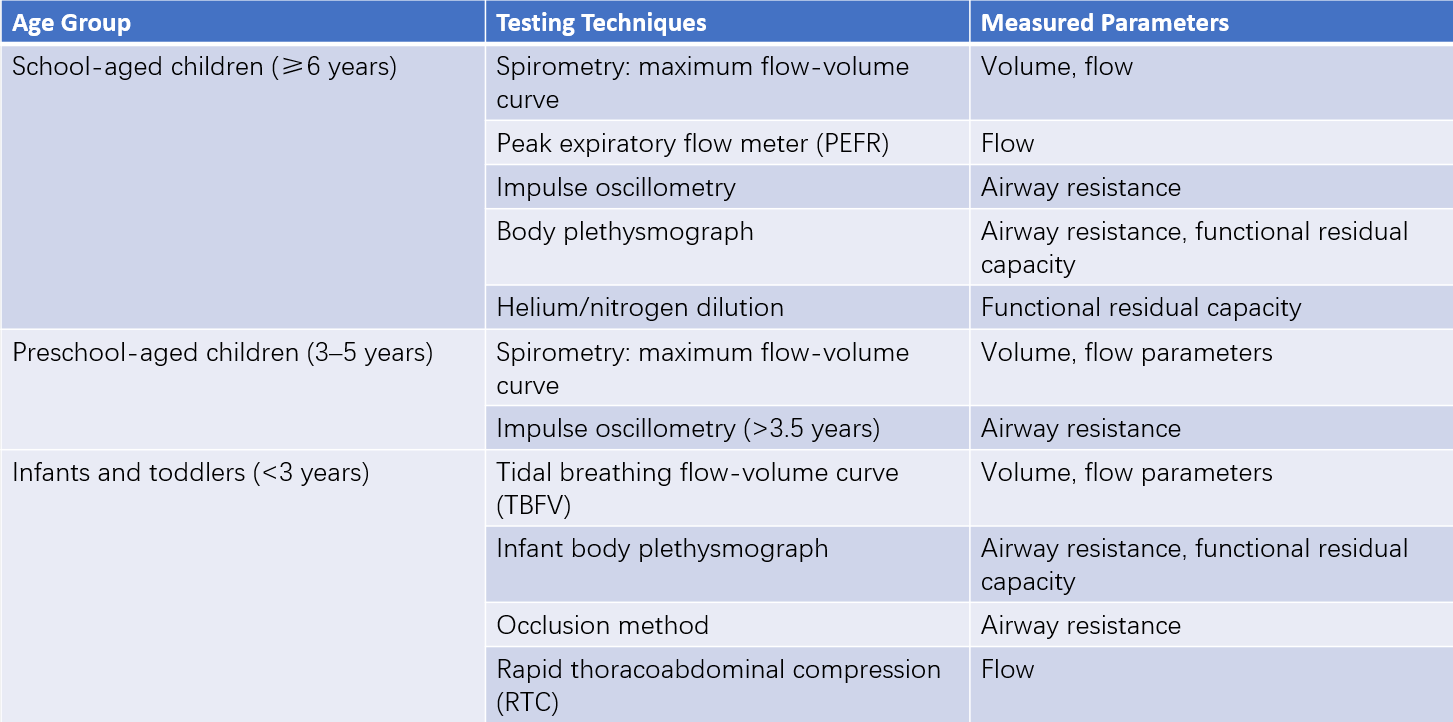
Table 2 Pulmonary function testing techniques and parameters by age group
Thoracoscopy
Thoracoscopy involves the use of a metal tube equipped with a light source, which is introduced into the thoracic cavity via an incision in the chest wall. This technique enables observation of pleural and pulmonary lesions and treatment of certain pleural diseases. In addition, thoracoscopy is useful for diagnosing and managing mediastinal and pericardial diseases as well as thoracic trauma.
Thoracentesis and Closed Thoracic Drainage
Thoracentesis, often referred to as "chest tap," is a procedure used to aspirate pleural fluid or air through a needle inserted into the thoracic cavity, primarily for diagnostic and therapeutic purposes in cases of pleural effusion or pneumothorax. Closed thoracic drainage, also known as "thoracostomy," is a procedure mainly used for the treatment of empyema, traumatic hemothorax, tension pneumothorax, and large-volume pleural effusions.