Acquired Immunodeficiency Syndrome (AIDS) is an infectious disease caused by the Human Immunodeficiency Virus (HIV). It is highly contagious and associated with a very high mortality rate.
Etiology
HIV belongs to the RNA retroviruses family and has a diameter of 100–200 nm. Currently, two types of HIV have been identified: HIV-1 and HIV-2. Both can lead to AIDS, although HIV-2 has weaker pathogenicity compared to HIV-1. HIV-1 includes nine subtypes (A, B, C, D, E, F, G, H, and O), with subtype B being the most common. The virus is spherical or elliptical in shape, with a lipid envelope containing serrated surface projections. It has a cylindrical core that contains magnesium-dependent reverse transcriptase. HIV consists of structural proteins such as P19, core proteins P24 and P15, reverse transcriptase proteins P66 and P51, envelope protein gp120, and transmembrane protein gp41. The virus is sensitive to heat and can be inactivated at 56°C for 30 minutes. It can also be inactivated by 50% ethanol, 0.3% hydrogen peroxide, 0.2% sodium hypochlorite, or 10% bleaching powder within 10 minutes. However, the virus exhibits resistance to formaldehyde solution, ultraviolet radiation, and gamma rays.
Epidemiology
HIV infection in children is typically transmitted from adults. The first case of pediatric HIV infection was reported in 1982, and it is estimated that approximately 1,000 newborns with HIV are born globally every day. As of 2001, the Joint United Nations Programme on HIV/AIDS reported that, over the past 20 years, there were 56 million cumulative cases of HIV infection, 22 million deaths including 4.3 million children, and nearly 2 million children (aged 0–14) living with HIV by the end of 2022. The prevention of vertical transmission remains the most effective strategy to control HIV infection in infants and young children. With successful interventions, the risk of vertical transmission can be reduced to less than 2%, although such interventions remain inaccessible in many resource-limited countries. Despite significant progress in diagnosing and treating infant and pediatric HIV infections over the past decade, over 1,100 new infections in children under 15 occur globally each day, with 90% of cases occurring in developing countries.
HIV-infected newborns often develop clinical symptoms within the first year of infection. It is estimated that one-third of infected children die by the age of one year, and nearly half may face death by the age of two if effective treatment is not provided.
Sources of Infection
Patients and asymptomatic carriers of the virus serve as the primary sources of infection, particularly the latter. The virus is predominantly found in blood, semen, uterine secretions, and vaginal secretions. Other bodily fluids such as saliva, tears, and breast milk also contain the virus and have infectious potential.
Modes of HIV Transmission in Children
Vertical Transmission
This is the main route of infection in children. Infected pregnant women can transmit the virus to their infants through the placenta, during delivery, or postpartum via bloody secretions or breastfeeding.
Bloodborne Transmission
Cases have been linked to activities such as blood transfusion, injection, or organ transplantation.
Other Routes
While sexual transmission and artificial insemination are primarily observed in adults, these modes of transmission occur less commonly in children.
Current evidence does not support the transmission of HIV through air, insects, water, food, or general contact with AIDS patients, such as handshakes, shared swimming pools, or bedding. Incidental contact leading to infection has also not been reported.
Pathogenesis
HIV produces reverse transcriptase, which uses viral RNA as a template to generate complementary DNA (cDNA). This cDNA integrates into the host cell's DNA, allowing the virus to replicate during the host cell's DNA replication. Within 1–2 weeks of infecting target cells, the virus buds off from the original cells and invades new target cells, leading to the destruction of CD4+ T lymphocytes in the body. Research in recent years has revealed that when HIV invades CD4+ T lymphocytes, it relies on a viral fusion protein (fusin). This promotes the fusion of CD4+ T lymphocytes, causing uninfected and infected cells to merge and become directly damaged. The massive destruction of CD4+ T lymphocytes impairs the ability of these cells to assist B lymphocytes with differentiation, resulting in abnormal humoral immune function. This manifests as hyperimmunoglobulinemia, the presence of autoantibodies, and reduced responsiveness to new antigens. Defective antibody responses make children prone to severe pyogenic infections. Impairments or failures in cell-mediated immunity lead to various opportunistic infections, such as infections caused by Mycobacterium tuberculosis, Pneumocystis jirovecii, Listeria monocytogenes, and cytomegalovirus. These infections are common causes of death.
Pathology
Post-HIV infection, pathological changes may occur in immune organs such as lymph nodes and the thymus. Lymph nodes exhibit two types of changes: reactive changes and neoplastic changes. In the early stages, reactive lymphoid hyperplasia is observed, followed by angioimmunoblastic lymphadenopathy-like changes. Subsequently, lymphocytes within the lymph nodes become sparse, with germinal centers appearing empty. In the spleen, the T-cell zones surrounding the small splenic arteries and splenic lymphoid follicles exhibit lymphocyte depletion, with germinal centers absent or completely lacking lymphoid components. Severe epithelial atrophy is observed in the thymus, accompanied by a lack of Hassall's corpuscles. Opportunistic infections are common and severe in children with AIDS, with pathological changes varying depending on the specific pathogen. HIV frequently involves the central nervous system, leading to changes such as gliosis, focal necrosis, perivascular inflammatory infiltration, formation of multinucleated giant cells, and demyelination.
Clinical Manifestations
The occurrence and progression of symptoms and signs in infected children depend on the level of immune system damage and the functional status of the organ systems in the body. In 1994, the United States Centers for Disease Control and Prevention (CDC) classified HIV infection based on clinical manifestations and immunological status. Clinically, HIV infection is divided into: asymptomatic (N), mild symptoms (A), moderate symptoms (B), and severe symptoms (C). Immunologically, it is categorized into: no immunosuppression (N1, A1, B1, C1), moderate immunosuppression (N2, A2, B2, C2), and severe immunosuppression (N3, A3, B3, C3).
Asymptomatic (N)
Children exhibit no infection symptoms or signs, or present with only one mild clinical condition.
Mild Symptoms (A)
Children show at least two or more of the following signs without meeting the criteria for moderate or severe symptoms: lymphadenopathy (>0.5 cm, involving more than two sites, bilaterally symmetrical), hepatomegaly, splenomegaly, dermatitis, parotitis, recurrent or persistent upper respiratory tract infections, sinusitis, or otitis media.
Moderate Symptoms (B)
In addition to the conditions listed under A, children exhibit one or more of the following:
- Anemia (Hb < 80 g/L), neutropenia (<1 × 109/L), or thrombocytopenia (<100 × 109/L) lasting for more than 30 days.
- Bacterial meningitis, pneumonia, or septicemia with positive cultures.
- Oral candidiasis persisting for more than 2 months in infants under 6 months.
- Cardiomyopathy.
- Cytomegalovirus infection occurring within the first month of life, recurrent or chronic diarrhea, or hepatitis.
- Herpes simplex virus (HSV) infections causing oral ulcers with more than two episodes in one year, or HSV bronchiolitis, pneumonia, or esophagitis occurring within the first month of life.
- Herpes zoster infection with at least two episodes or involving multiple sites.
- Smooth muscle tumors associated with Epstein-Barr virus. Interstitial lymphoid pneumonia or pulmonary lymphoid hyperplasia syndrome.
- Nephropathy.
- Nocardiosis or fever persisting for more than 1 month.
- Toxoplasmosis occurring within the first month of life.
- Disseminated varicella.
Severe Symptoms (C)
These include:
Severe recurrent bacterial infections, including sepsis, pneumonia, meningitis, bone or joint infections, and deep abscesses, excluding otitis media, superficial mucocutaneous abscesses, or infections secondary to catheterization.
Candidiasis involving the esophagus, trachea, bronchi, or lungs; deep fungal infections with systemic dissemination (beyond pulmonary or mediastinal lymph nodes).
Cryptosporidiosis causing diarrhea persisting for more than 1 month.
Cytomegalovirus infections occurring beyond the first month of life, involving sites beyond the liver, spleen, or lymph nodes.
Encephalopathy with at least one of the following symptoms persisting for over 2 months without other identifiable causes:
- Developmental regression or cognitive decline.
- Impaired brain development, evidenced by acquired microcephaly or CT/MRI-documented brain atrophy.
- Acquired motor dysfunction, such as paralysis, pathological reflexes, ataxia, or impaired fine motor skills. At least two such signs are required.
Herpes simplex virus-induced mucosal ulcers persisting for more than 1 month, or HSV bronchitis, pneumonia, or esophagitis occurring beyond the first month of life.
Histoplasmosis with involvement beyond pulmonary or mediastinal lymph nodes.
Kaposi's sarcoma or lymphoma (e.g., Burkitt lymphoma, immunoblastic lymphoma, B-cell lymphoma, or those of unknown immunophenotype).
Extrapulmonary disseminated tuberculosis.
Pneumocystis pneumonia.
Progressive multifocal leukoencephalopathy.
Nontyphoidal salmonella septicemia with recurrent episodes.
Toxoplasmosis involving the central nervous system, occurring beyond the first month of life.
Wasting syndrome characterized by the following:
- Persistent loss of at least 10% of baseline body weight.
- A decline of 25 percentiles in weight-for-age for children over 1 year old.
- A decline of 5 percentiles in weight-for-height post 1 month of age. This is often accompanied by:
- Chronic diarrhea (at least two episodes of loose stools per day, persisting for over 1 month).
Persistent or intermittent fever lasting for over 1 month.
Laboratory Tests
Pathogen Diagnosis
Viral Antibody Testing
This serves as the primary method for initial screening.
- Screening Tests: Enzyme-linked immunosorbent assay (ELISA) using serum or urine, and rapid blood tests.
- Confirmatory Tests: Western blot or immunofluorescence assay. Detection of viral antibodies has limitations for diagnosing children under 18 months of age.
Virus Isolation
A common method involves co-culturing peripheral blood mononuclear cells (PBMC) from the tested individual with phytohemagglutinin (PHA)-stimulated normal human PBMCs (with added IL-2 at 10 U/ml) over 3 days. After 3 weeks, cytopathic effects, reverse transcriptase activity, P24 antigen, or viral RNA (via PCR) are assessed to determine the presence of HIV. This method is generally used for research purposes and not as a diagnostic criterion.
Antigen Detection
This primarily focuses on detecting the P24 core antigen, which can typically be identified within 1–2 weeks of infection.
Viral Nucleic Acid Testing
Small quantities of viral nucleic acids can be detected using PCR or ligase chain reaction (LCR) techniques.
Diagnostic Tests for Immunodeficiency
Analysis of Peripheral Blood Lymphocyte Subsets
Reversal of the CD4+/CD8+ ratio, reduced natural killer (NK) cell activity, diminished or absent delayed-type hypersensitivity skin responses, and positive results for anti-lymphocyte, anti-sperm, or antinuclear antibodies can be seen. Elevated β2-microglobulin levels and increased urinary neopterin concentrations are also observed.
Pathogen Identification in Opportunistic Infections:
Early detection is crucial to clearly identify the causative pathogen and initiate targeted treatment.
Diagnosis
The current early diagnostic strategy for infants involves collecting the first blood sample at six weeks after birth. If the first sample tests positive, a second blood sample is collected promptly for confirmation. If both samples test positive, the result is reported as "positive for the early diagnosis of HIV infection in infants," and the child is diagnosed with HIV infection.
The diagnostic criteria for pediatric HIV infection and AIDS are as follows:
Asymptomatic HIV Infection in Children
Epidemiological History:
- Infants born to HIV-infected mothers.
- History of transfusions with unscreened blood or blood products.
Clinical Manifestations: No symptoms or signs are present.
Laboratory Tests:
- For children ≥18 months, HIV antibody tests are positive and confirmed by confirmatory tests.
- Plasma HIV RNA is positive.
Diagnostic Criteria:
- For children aged ≥18 months, the presence of an epidemiological history and any positive laboratory test confirms the diagnosis.
- For children <18 months, the presence of an epidemiological history and positive HIV RNA results from two separate plasma samples confirm the diagnosis.
AIDS in Children
Epidemiological History: Identical to that of asymptomatic HIV infection.
Clinical Manifestations:
- Persistent unexplained generalized lymphadenopathy (>1 cm in diameter), hepatosplenomegaly, or parotitis.
- Persistent unexplained fever lasting for more than 1 month.
- Chronic recurrent diarrhea.
- Delayed growth and development.
- Significant weight loss (>10% of baseline weight within 3 months).
- Protracted and unresolving interstitial pneumonia and oral fungal infections.
- Frequent opportunistic infections.
Compared to adult AIDS, pediatric AIDS has the following characteristics:
- Shorter latency period, acute disease onset, and rapid progression after HIV infection.
- Growth failure deviating from normal growth curves is a unique feature in pediatric HIV infection.
- Increased susceptibility to recurrent bacterial infections, particularly to encapsulated bacteria.
- Chronic parotitis and lymphoid interstitial pneumonia are common.
- Infants are highly prone to encephalopathy, which manifests early, progresses rapidly, and has a poor prognosis.
Laboratory Tests:
- HIV antibody positivity confirmed by confirmatory tests and plasma HIV RNA positivity.
- Reduced total CD4+ T lymphocyte count and percentage of CD4+ T lymphocytes among total lymphocytes in peripheral blood (Table 7-5).
Diagnostic Criteria:
- Children presenting with one or more clinical manifestations, and for those ≥18 months, HIV antibody positivity (confirmed by confirmatory tests) or HIV RNA positivity.
- For children <18 months, HIV RNA positivity from two separate samples confirms the diagnosis.
- CD4+ T-cell counts and percentages should be assessed, if possible, to evaluate immune status.
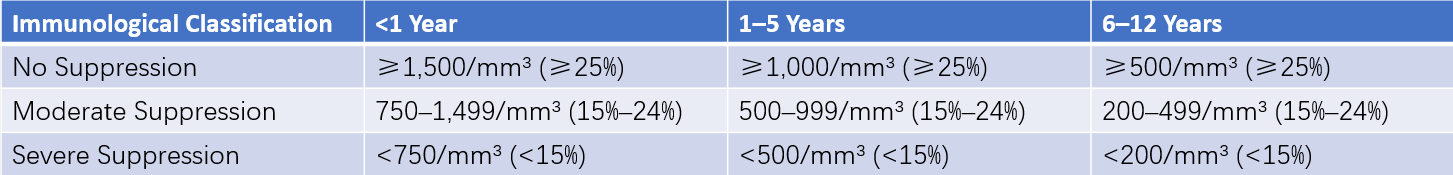
Table 1 Classification of immunological status Based on CD4+ cell count and CD4+ T cell percentage in pediatric AIDS patients
Treatment
Indications for Antiretroviral Therapy
Advances in the understanding of the pathogenesis of HIV infection and the introduction of new antiretroviral drugs have significantly changed the approach to HIV treatment. All antiretroviral drugs can be used for pediatric patients. The current indications for initiating antiretroviral therapy include clinical symptoms of HIV infection, corresponding to clinical categories A, B, or C; a decline in the absolute count or percentage of CD4+ T cells to levels indicative of moderate or severe immunosuppression; infants under the age of one, regardless of their clinical, immunological, or viral load status. For children above one year of age with no clinical symptoms, early treatment is generally recommended unless there is clear evidence of very low risk of disease progression or other factors necessitating a delay in therapy. Close monitoring of the clinical, immunological, and viral load status is essential for patients who have not yet initiated treatment.
Therapy is initiated upon observing conditions such as extremely high or progressively increasing HIV RNA levels, a rapid decline in the absolute count or percentage of CD4+ T cells resulting in moderate immunosuppression, or the appearance of clinical symptoms.
Antiviral Therapy
Nucleoside Reverse Transcriptase Inhibitors
Examples include zidovudine (AZT), didanosine (DDI), lamivudine (LAM), and stavudine (d4T). These drugs selectively bind to HIV reverse transcriptase and incorporate into the growing DNA chain, causing termination of DNA replication and thereby inhibiting HIV replication and transcription.
Non-Nucleoside Reverse Transcriptase Inhibitors
Examples include nevirapine (NVP) and delavirdine (DLR). These drugs act on specific sites of the HIV reverse transcriptase enzyme, causing it to lose its activity and thereby inhibiting HIV replication.
Protease Inhibitors
Examples include saquinavir, indinavir (IDV), nelfinavir, and ritonavir. They act by inhibiting the protease enzyme, thereby blocking the synthesis of proteins necessary for HIV replication and maturation, ultimately suppressing HIV replication.
The use of a single drug is associated with poor efficacy; therefore, combined therapy with two or more drugs is advocated. However, there is no consensus on the optimal drug combinations. Children diagnosed with AIDS should receive treatment at designated medical facilities.
Immunological Therapy
Recombinant IL-2 in conjunction with antiviral medications has demonstrated benefits in improving immune function. IL-12 is another cytokine with therapeutic value, and in vitro studies indicate that IL-12 can enhance the capability of immune cells to kill HIV-infected cells.
Supportive and Symptomatic Treatment
Measures include blood transfusions, nutritional support, and supplementation with vitamins, particularly vitamin B12 and folic acid.
Anti-Infection and Anti-Tumor Therapy
Appropriate therapies should be provided in cases of infection or tumor development.
Prevention
Special considerations should be made in the prevention of pediatric AIDS:
- Dissemination of knowledge about AIDS to reduce the rate of HIV infection among women of reproductive age.
- HIV-infected individuals should avoid pregnancy. HIV-infected or AIDS-affected pregnant women should be counseled to terminate the pregnancy or undergo cesarean delivery whenever possible.
- Members of high-risk populations should strictly be prohibited from donating blood, and HIV antibody-positive individuals must be excluded from blood donor pools.
- HIV-positive mothers and their newborns should receive AZT to reduce the probability of vertical transmission.
- Strict quality control of blood and blood-derived products must be enforced.
- Vaccine Prevention: The AIDS VAX vaccine, developed using genetic recombination technology targeting the HIV-1 glycoprotein gp120, is currently undergoing Phase III clinical trials.