Retinopathy of prematurity (ROP) is an abnormal proliferative vascular disease of the retina that occurs in premature infants. Severe cases may result in visual impairment. Studies have shown that the incidence of ROP is 65.8% in premature infants with a birth weight of less than 1,251g, and 81.6% in those with a birth weight of less than 1,000g. ROP accounts for approximately 6%–18% of childhood blindness, underscoring the importance of prevention and treatment efforts.
Etiology and Risk Factors
Prematurity
Prematurity is the fundamental cause of ROP. The lower the gestational age and the lower the birth weight, the higher the incidence and severity of ROP.
Genetic and Hereditary Factors
There is significant individual variation in ROP occurrence, which may be related to specific genetic predispositions.
Oxygen Therapy
The role of oxygen therapy in causing ROP depends on several factors, including higher concentrations of supplemental oxygen, longer durations of oxygen use, and significant fluctuations in arterial oxygen tension.
Anemia and Blood Transfusion
Anemia and blood transfusions are associated with the occurrence and progression of ROP.
Metabolic Acidosis
Metabolic acidosis can promote retinal neovascularization, with longer durations of acidosis increasing the likelihood of new blood vessel formation.
Other Factors
Recurrent apnea, infections, and low PaCO2 are additional risk factors for ROP.
Clinical Features
The clinical manifestations of ROP primarily involve retinal abnormalities. Based on the International Classification of Retinopathy of Prematurity, the severity of retinal disease is categorized into five stages:
- Stage 1: A flat and thin white demarcation line appears between the vascularized posterior retina and the avascular peripheral retina.
- Stage 2: The white demarcation line becomes wider and elevated, forming a ridge protruding above the retinal surface.
- Stage 3: The ridge becomes more pronounced and appears pink. Fibrous proliferation may occur and extend into the vitreous.
- Stage 4: Partial retinal detachment takes place, which can be further classified based on macular involvement:
- Stage 4a: Peripheral retinal detachment without macular involvement.
- Stage 4b: Retinal detachment involving the macula.
- Stage 5: Total retinal detachment typically forms a funnel-shaped appearance, which can be further categorized into four types: wide, narrow, anterior wide and posterior narrow, and anterior narrow and posterior wide. Extensive connective tissue proliferation and the formation of fibrovascular membranes behind the lens often occur in this stage.
In addition to these stages, specific pathological changes are characteristic of ROP:
- Plus Disease (Plus ROP): This is characterized by severe dilation and tortuosity of the posterior retinal vessels or marked dilation of anterior iris vessels. Plus disease indicates active ROP and is associated with a poor prognosis. The presence of plus disease is denoted with a "+" next to the stage (e.g., Stage 3+).
- Threshold Disease (Threshold ROP): This refers to Stage 3 ROP located in Zone I or Zone II, with neovascularization occupying five contiguous clock hours or a cumulative eight total clock hours of involvement, along with the presence of plus disease. This stage is critical for early treatment intervention.
- Prethreshold Disease (Prethreshold ROP): Prethreshold ROP includes two categories:
- Disease limited to Zone I, ranging from Stage 1 to Stage 3 ROP.
- Disease located in Zone II, which may present as: Stage 2 ROP with plus disease, Stage 3 ROP without plus disease, or Stage 3 ROP with plus disease but neovascularization covering fewer than five contiguous clock hours or a cumulative eight total clock hours.
- Aggressive Posterior ROP (APROP): This form of ROP is confined to Zone I and exhibits linear neovascularization patterns. APROP progresses rapidly and requires heightened vigilance.
Screening for ROP
Early diagnosis of retinopathy of prematurity (ROP) primarily relies on systematic screening. Establishing a screening protocol and performing fundus examinations at appropriate times are essential for early detection, diagnosis, and intervention for ROP.
Screening Criteria and Indications
The targets for ROP screening include all premature infants with a gestational age of ≤34 weeks or a birth weight of <2,000g.
Timing of Screening
The timing for the initial screening depends on both postnatal age and corrected gestational age (CGA). Corrected gestational age correlates more closely with the onset of severe ROP, with lower gestational ages at birth being associated with later onset. The relationship between gestational age, postnatal age, CGA, and initial ROP screening guides the decision on the first screening’s timing.
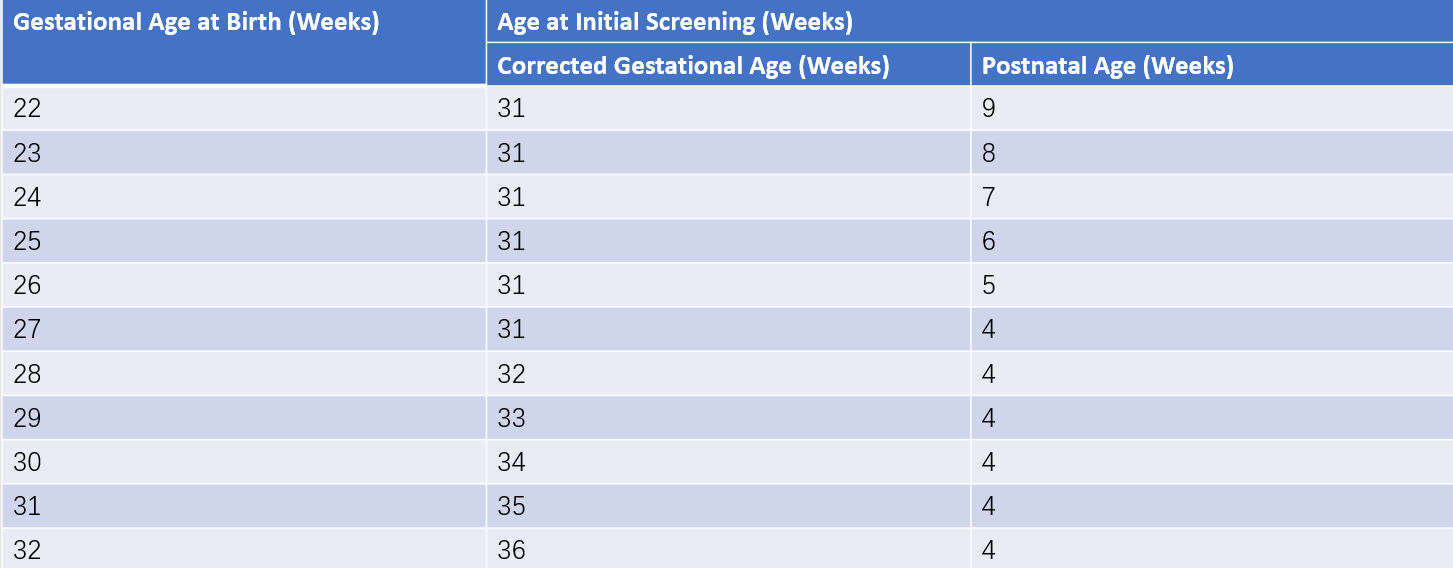
Table 1 Timing of initial screening based on gestational age at birth (unit: weeks)
Examination Methods
Two methods are commonly used for screening: digital retinal cameras and indirect ophthalmoscopy.
- Digital Retinal Cameras: Advanced digital retinal cameras are increasingly adopted in hospitals. A small amount of gel is applied to the camera lens, which is then brought into contact with the infant’s eye to capture images of the retina in five directions (central, superior, inferior, left, and right). The images are stored electronically, can be printed, and may be remotely transmitted to experienced ophthalmologists for evaluation.
- Indirect Ophthalmoscopy: In the absence of a retinal camera, an indirect ophthalmoscope with a 25D or 28D lens is used for fundus examination. Indirect ophthalmoscopy, however, is subjective and prone to missed diagnoses, requiring a high level of expertise from the examiner.
Follow-Up
Follow-up frequency and duration are determined by the initial screening results. Evaluations are performed by an ophthalmologist and continue until the corrected gestational age reaches term and the retina achieves complete vascularization.
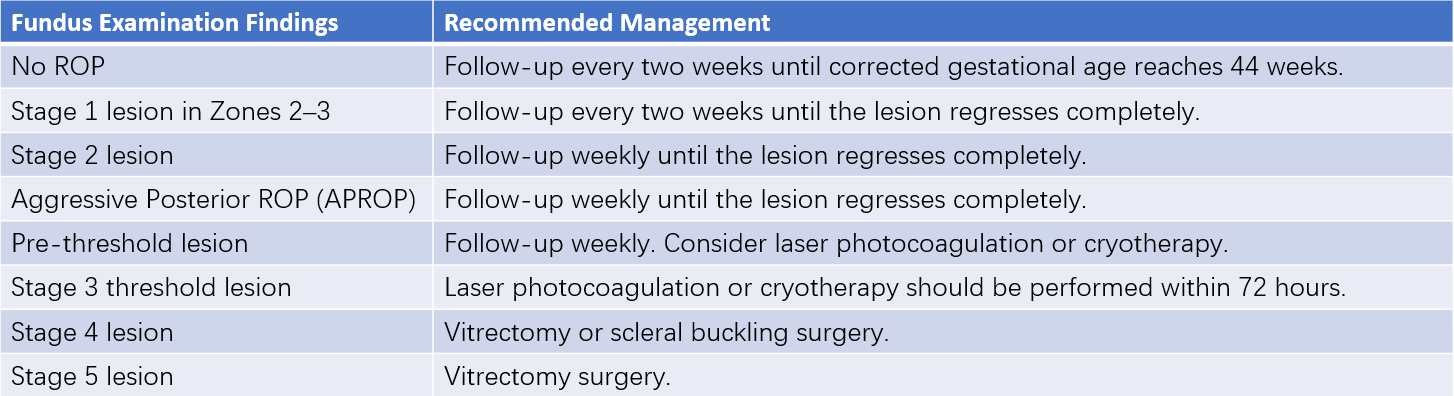
Table 2 Fundus follow-up and management recommendations for premature infants with ROP
Treatment
Once Stage 3 ROP is diagnosed through screening, treatment is initiated promptly. Current treatments primarily involve medications, laser therapy, and surgery, though laser and surgical interventions may cause varying degrees of retinal damage. Post-treatment, retinal vascular development typically halts, which may lead to impaired vision.
Pharmacological Treatment
Medical management of ROP focuses on intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF) antibodies.
Laser Photocoagulation
Early ROP responds well to laser therapy, achieving better outcomes for Zone I ROP compared to cryotherapy, with similar efficacy for Zone II disease. Laser photocoagulation offers greater precision and reduces complications such as vitreous hemorrhage, postoperative conjunctival edema, and intraocular inflammation. It is considered the treatment of choice for threshold ROP.
Cryotherapy
Cryotherapy is conducted under local anesthesia or general anesthesia. During the procedure, 40–50 cryotherapy spots are applied to the retina through the conjunctiva under the guidance of an indirect ophthalmoscope. Cryotherapy is generally reserved for threshold ROP.
Scleral Buckling
For cases where threshold ROP progresses to Stage 4 or early Stage 5 (with some visibility of the fundus), scleral buckling is used to relieve retinal traction, facilitate the absorption of subretinal fluid, and achieve retinal reattachment, thereby halting progression to Stage 5.
Vitrectomy Surgery
In cases where scleral buckling fails or for advanced Stage 5 ROP, complex vitrectomy is performed. Postoperatively, partial or complete anatomical retinal reattachment may be achieved, but restoration of functional vision is rare.
Prevention
Management of Neonatal Complications
Preventing and treating complications in premature infants reduces the severity of illness and minimizes the risk of ROP. Higher rates of complications and severity increase the likelihood of developing ROP.
Standardized Oxygen Therapy
Efforts focus on reducing oxygen concentration levels, shortening the duration of oxygen therapy, and minimizing fluctuations in arterial oxygen tension.
Additional Measures
Prevention and treatment strategies include managing apnea, correcting metabolic acidosis, preventing anemia and limiting blood transfusions, addressing infections, and avoiding excessively low PaCO2 levels.