Neonatal asphyxia refers to a condition in which a newborn is unable to establish normal spontaneous breathing after birth, leading to hypoxemia, hypercapnia, and multi-organ injury. It is one of the significant causes of neonatal mortality and childhood disability.
Etiology
The fundamental cause of asphyxia is hypoxia. Any factor that disrupts gas exchange in fetuses or newborns can lead to asphyxia. While it may occur during pregnancy, most cases develop after the onset of labor. Neonatal asphyxia often represents the continuation of fetal asphyxia (intrauterine distress).
Maternal Factors
These include:
- Chronic or severe maternal conditions, such as cardiopulmonary insufficiency, severe anemia, diabetes, or hypertension.
- Pregnancy complications, including hypertensive disorders during pregnancy.
- Maternal substance abuse, smoking (including passive smoking), advanced maternal age (≥35 years), very young maternal age (<16 years), or multiple pregnancies.
Placental Factors
These include placenta previa, placental abruption, or placental aging.
Umbilical Cord Factors
These include compression, prolapse, nuchal cord, knots, excessively short cord, or traction of the umbilical cord.
Fetal Factors
These include:
- Premature infants or macrosomic infants.
- Congenital anomalies, such as esophageal atresia, laryngeal web, underdeveloped lungs, or congenital heart diseases.
- Intrauterine infections.
- Airway obstructions, such as aspiration of amniotic fluid or meconium.
Delivery-Related Factors
These include cephalopelvic disproportion, uterine inertia, breech presentation, use of obstetric forceps or vacuum extraction, or exposure to anesthetics, analgesics, or oxytocic medications during labor.
Pathophysiology
Obstruction of the Transition from Fetal to Neonatal Respiratory and Circulatory Functions
In normal circumstances, the transition of fetal respiratory and circulatory systems to neonatal functions involves the following: clearance of fetal lung fluid, secretion of pulmonary surfactant, establishment of functional residual capacity in the alveoli, reduction in pulmonary vascular resistance, increase in systemic vascular resistance, and functional closure of the ductus arteriosus and foramen ovale. In neonates with asphyxia, normal breathing cannot be established, leading to an inability to expand the alveoli and clear lung fluid. Hypoxia and acidosis impair surfactant production and activity, increase pulmonary vascular resistance, and cause persistent fetal circulation, resulting in persistent pulmonary hypertension. This further exacerbates tissue hypoxia, ischemia, and acidosis, ultimately leading to irreversible multi-organ hypoxic and ischemic injury.
Ischemic Changes in Organs During Asphyxia
In the early stages of asphyxia, hypoxia and acidosis elicit the classic "diving reflex," leading to a redistribution of blood flow. Blood vessels in non-essential organs, such as the lungs, intestines, kidneys, muscles, and skin, constrict, reducing blood supply to these organs to preserve blood flow to vital organs such as the brain, heart, and adrenal glands. Simultaneously, the secretion of hormones such as ACTH, corticosteroids, catecholamines, renin, and atrial natriuretic peptides increases, enhancing myocardial contractility, heart rate, cardiac output, and peripheral blood pressure to maintain brain and heart perfusion. However, prolonged hypoxemia consumes glycogen stores, exacerbates anaerobic metabolism, and worsens metabolic acidosis. Over time, blood flow to the brain, heart, and adrenal glands decreases, myocardial function deteriorates, heart rate and arterial blood pressure drop, and organ perfusion diminishes, culminating in multi-organ damage.
Changes in Respiration
Primary Apnea
In the early stages of fetal or neonatal hypoxia, compensatory breathing deepens and accelerates. If hypoxia is not corrected, breathing ceases, and the heart rate slows, leading to primary apnea. During this stage, muscle tone is preserved, blood pressure may rise slightly, and cyanosis is present. This stage typically resolves with the clearance of the airway and physical stimulation.
Secondary Apnea
If hypoxia persists, the newborn may exhibit several deep gasping respirations before experiencing cessation of breathing, resulting in secondary apnea. During this stage, muscle tone is lost, and heart rate, blood pressure, and oxygen saturation levels continue to decline. Positive pressure ventilation is necessary to restore spontaneous respiration at this point; otherwise, the condition can become life-threatening.
Distinguishing between primary and secondary apnea can be challenging in clinical settings. For this reason, management should proceed as secondary apnea to avoid delays in interventions.
Biochemical and Metabolic Changes in Blood
Reductions in PaO2 and pH and the Development of Mixed Acidosis
These changes occur due to anaerobic metabolism and airway obstruction associated with hypoxia.
Glucose Metabolism Disorders
Catecholamine and glucagon secretion increase early in asphyxia, leading to normal or elevated blood glucose levels. This is followed by glycogen depletion, resulting in hypoglycemia.
Hyperbilirubinemia
Acidosis impairs bilirubin metabolism and its binding to albumin, reducing hepatic enzyme activity and increasing the risk of hyperbilirubinemia.
Hyponatremia and Hypocalcemia
Dilutional hyponatremia occurs due to abnormal secretion of atrial natriuretic peptide and antidiuretic hormone. Hypoxia-related parathyroid dysfunction, calcium channel opening, and calcium influx contribute to the development of hypocalcemia.
Clinical Manifestations
Fetal Distress in Utero
Early signs include increased fetal movements and a heart rate ≥160 beats per minute. Late-stage manifestations may include decreased or absent fetal movements, a heart rate <100 beats per minute, and meconium-stained amniotic fluid.
Assessment Using Apgar Scores
Apgar scoring was introduced in 1953 by Dr. Virginia Apgar, an anesthesiologist, and is internationally recognized as the simplest and most practical method for evaluating neonatal asphyxia. The score consists of five indicators: skin color (appearance), heart rate (pulse), response to stimulation (grimace), muscle tone (activity), and respiratory effort (respiration). Each parameter is scored from 0 to 2 points, with a maximum total of 10 points. Assessments are performed at 1 minute, 5 minutes, and 10 minutes after birth, and in neonates requiring continued resuscitation, scores may be assessed at 15 and 20 minutes. Scores of 8–10 reflect normal status, 4–7 indicate mild asphyxia, and 0–3 denote severe asphyxia. One-minute scores reflect the severity of asphyxia, while the five-minute scores provide information about the efficacy of resuscitation and help predict prognosis.
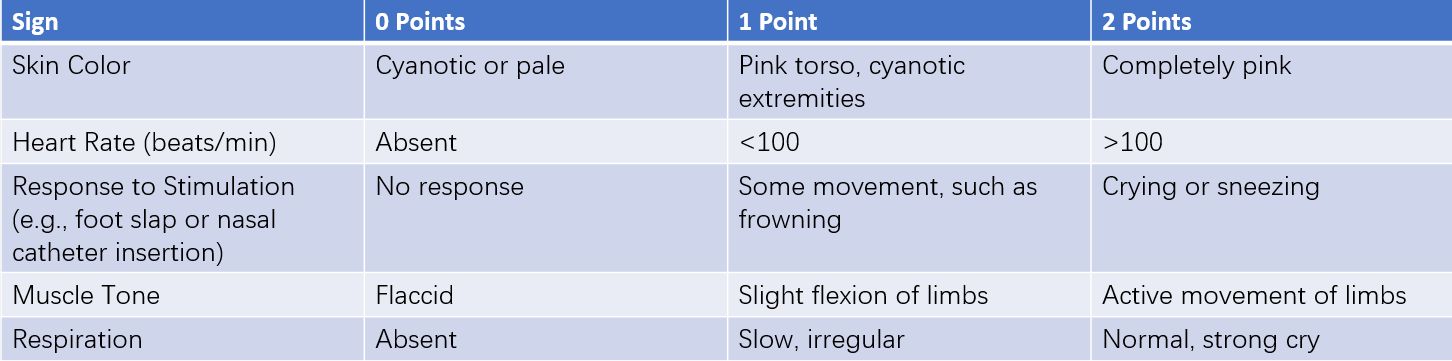
Table 1 Neonatal Apgar scoring criteria
Symptoms of Multi-Organ Injury
Hypoxia and ischemia can cause damage to multiple organs, although different tissues vary in their sensitivity to oxygen deprivation. Brain cells are the most sensitive, followed by myocardial cells, liver cells, and adrenal gland cells. Fibrous tissue, epithelial cells, and skeletal muscle cells are more resistant, resulting in differences in the frequency and severity of organ damage:
- Central Nervous System: Hypoxic-ischemic encephalopathy and intracranial hemorrhage.
- Respiratory System: Meconium aspiration syndrome, pulmonary hemorrhage, and respiratory distress syndrome.
- Cardiovascular System: Persistent pulmonary hypertension of the newborn and hypoxic-ischemic myocardial disease, with manifestations such as arrhythmias, heart failure, and cardiogenic shock.
- Renal System: Impairments like renal insufficiency, acute kidney failure, and renal vein thrombosis.
- Metabolic System: Disorders like hypoglycemia or hyperglycemia, hypocalcemia, hyponatremia, hypercapnia, and prolonged or worsened jaundice.
- Digestive System: Conditions such as stress-induced ulcers or necrotizing enterocolitis.
- Hematologic System: Disseminated intravascular coagulation (DIC), often appearing within hours or days after birth, and thrombocytopenia, which may be caused by ischemic damage to the bone marrow and resolve gradually after 5–7 days.
Diagnosis
Currently, neonatal asphyxia diagnosis primarily relies on the Apgar scoring system. However, many researchers argue that Apgar scores alone should not be used as the sole criterion for evaluating asphyxia or predicting long-term neurological outcomes, particularly in cases involving prematurity, severe neonatal illness, or maternal use of sedatives.
To address these concerns, the American Academy of Pediatrics (AAP) and the American College of Obstetricians and Gynecologists (ACOG) jointly issued diagnostic criteria for neonatal asphyxia in 1996. These include:
- Severe metabolic or mixed acidosis in umbilical arterial blood gas analysis, with a pH <7.0.
- An Apgar score of 0–3, persisting for more than 5 minutes.
- Early neurological manifestations in neonates, such as seizures, coma, or hypotonia.
- Evidence of multi-organ dysfunction in the early neonatal period.
Auxiliary Examinations
For fetuses suspected of in-utero hypoxia, blood gas analysis can be performed on scalp blood during labor to assess the extent of hypoxia. After birth, evaluations of arterial blood gas, blood glucose, electrolytes, blood urea nitrogen, and creatinine levels may be conducted to assess biochemical abnormalities.
Treatment
Preparation for neonatal resuscitation before delivery includes prenatal consultation, coordination of the resuscitation team, and readiness of necessary equipment. Evaluation and resuscitation should immediately follow birth rather than being delayed until the 1-minute Apgar score is determined. Obstetricians, pediatricians, midwives, and anesthesiologists collaborate in the resuscitation process.
Resuscitation Protocols
The globally recognized ABCDE protocol is employed during resuscitation:
- A (Airway): Establishing a clear airway.
- B (Breathing): Facilitating normal respiration.
- C (Circulation): Ensuring proper cardiac function and circulation.
- D (Drugs): Administering appropriate medications.
- E (Evaluation): Continuously assessing the neonate's status.
The first three steps (A, B, and C) are considered the most crucial. Establishing an airway (A) is fundamental, breathing (B) is key, and evaluation (E) continues throughout the entire resuscitation process. Respiratory effort, heart rate, and oxygen saturation levels are the three principal indicators in resuscitation, following an ongoing cycle of evaluation, decision-making, and action until resuscitation is complete.
Resuscitation steps must follow the sequence of A → B → C → D without deviation. Most neonates recover through steps A and B, while fewer require A, B, and C. Only a very small proportion necessitate A, B, C, and D for successful resuscitation.
###Resuscitation Steps and Procedures
Based on the ABCDE resuscitation protocol, the process includes the following steps:
Rapid Assessment
A quick assessment lasting a few seconds is performed immediately after birth, focusing on:
- Whether the infant is full-term.
- Whether the amniotic fluid is clear.
- Whether muscle tone is good.
- Whether crying or breathing is adequate.
If any of these criteria are unmet, initial resuscitation is undertaken.
Initial Resuscitation
Warming
The delivery room temperature is maintained at 24–26°C. All newborns require drying of the head and body to maintain warmth. For full-term infants, a pre-warmed towel is used to wrap and dry the baby before placing them on a radiant warmer. Preterm infants with a gestational age of <32 weeks and/or birth weight <1500 g are wrapped in a clean plastic wrap or bag below the neck or covered with a plastic sheet and placed under a radiant warmer.
Positioning
The newborn's head is positioned in slight extension to ensure optimal airflow for nasal inhalation.

Figure 1 Correct positioning
Airway Clearance
Routine suctioning of the mouth, nose, and pharynx is not recommended, as it may increase the risk of bradycardia and respiratory depression. If significant secretions are present and breathing is obstructed, secretions can be cleared using a suction bulb or suction catheter, prioritizing the mouth, followed by the nose. The depth and duration of suctioning should be limited to 10 seconds, and the suction pressure should remain below 100 mmHg. For meconium-stained amniotic fluid and a neonate with poor vitality (evidenced by no breathing or gasping, heart rate <100 bpm, or low muscle tone—any one of these factors), endotracheal intubation is performed within 20 seconds. Meconium is suctioned using an appropriate catheter, withdrawing the endotracheal tube while suctioning within 3–5 seconds. If the amniotic fluid is clear or if staining is observed but the newborn is vigorous, endotracheal suctioning can be avoided.
Drying
The newborn's entire body is dried quickly using a warm, dry towel.
Stimulation
Gentle tactile stimulation, such as tapping the sole of the foot or rubbing the infant's back twice, induces spontaneous breathing. These initial steps are completed within 30 seconds.
Positive Pressure Ventilation (PPV)
If the newborn exhibits apnea or gasping, or the heart rate remains <100 bpm, positive pressure ventilation is applied. Effective PPV is administered within the first minute of life. For both full-term and preterm neonates, PPV is guided by continuous pulse oximetry monitoring, and 3-lead electrocardiographic monitoring may also be considered. For full-term neonates and preterm neonates with a gestational age ≥35 weeks, resuscitation begins with 21% oxygen. For preterm neonates <35 weeks, oxygen concentrations between 21% and 30% are used, adjusted with an oxygen blender to achieve target oxygen saturation levels. Peak inspiratory pressure during ventilation ranges from 20–25 cmH2O (1.96–2.45 kPa), or up to 30 cmH2O (2.94 kPa) in severe cases. Ventilation is delivered at 40–60 breaths per minute (or 30 breaths per minute during chest compressions). Indicators of effective PPV include a rapid increase in heart rate, observable chest rise, audible breath sounds, and improved oxygen saturation. After 30 seconds of effective ventilation, if spontaneous breathing is established and the heart rate is ≥100 bpm, PPV is gradually reduced and discontinued. If breathing remains inadequate or the heart rate is <100 bpm, PPV is continued via a face mask or an endotracheal tube.
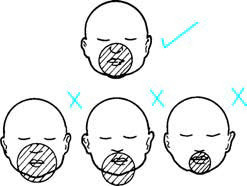
Figure 2 Mask positive pressure ventilation
Endotracheal Intubation
Intubation is performed under the following conditions:
- Meconium is visible during airway suctioning.
- PPV with a mask proves ineffective.
- Chest compressions are required.
- Certain medications (e.g., epinephrine, pulmonary surfactant) need to be administered via the endotracheal route.
- Specific cases such as congenital diaphragmatic hernia.
The size and depth of the endotracheal tube are determined based on the neonate's weight and gestational age.
Chest Compressions
If the heart rate remains <60 bpm after 30 seconds of effective PPV, chest compressions are initiated alongside continued PPV. Compressions are performed with both thumbs placed on the lower third of the sternum (just below the midpoint of the nipple line). The compression rate is 90 compressions per minute, with one breath delivered after every three compressions. Compression depth equals one-third of the anterior-posterior diameter of the chest. During compressions, PPV is delivered via an endotracheal tube, with the oxygen concentration increased to 100%. Heart rate assessment is conducted after 60 seconds of coordinated compressions and ventilation. If the heart rate is ≥60 bpm, compressions are discontinued, and PPV continues at a rate of 40–60 breaths per minute.
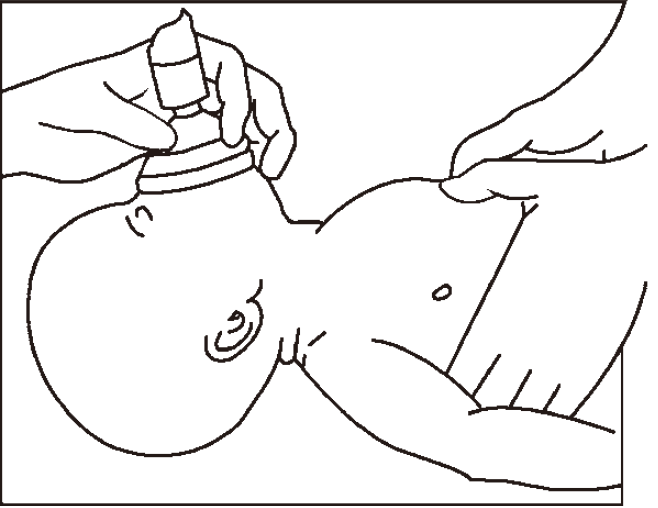
Figure 3 Positive pressure ventilation with resuscitation bag and mask, chest compressions using the two-thumb technique
Medication
Medications are rarely needed during neonatal resuscitation.
Epinephrine
If the heart rate remains <60 bpm after effective PPV and chest compressions for 60 seconds, a solution of 1:10,000 epinephrine is administered intravenously through an umbilical venous catheter at a dose of 0.1–0.3 ml/kg. If necessary, doses are repeated every 3–5 minutes. If umbilical venous access is not available, epinephrine may be administered endotracheally at a dose of 0.5–1.0 ml/kg, although repeat doses should be given via the intravenous route.
Volume Expanders
If the heart rate remains <60 bpm despite adequate PPV, chest compressions, and epinephrine, and signs of hypovolemia are present, an isotonic saline solution is administered intravenously at a dose of 5–10 ml/kg over 5–10 minutes. Repeated doses may be given as needed. In cases of significant blood loss, cross-matched compatible blood may be transfused.
Sodium Bicarbonate
The use of sodium bicarbonate is generally not recommended during resuscitation.
Post-Resuscitation Monitoring and Transport
After resuscitation, monitoring continues for temperature, respiration, heart rate, blood pressure, urine output, oxygen saturation, and potential multi-organ injuries resulting from asphyxia. For neonates with severe complications, transfer to a neonatal intensive care unit (NICU) is required. During transport, special attention is given to maintaining warmth, monitoring vital signs, and providing necessary treatment.
Prognosis
The prognosis significantly depends on the duration of asphyxia. Cases involving chronic in utero hypoxia, prolonged or inadequately managed severe asphyxia may lead to poor outcomes.
Prevention
This involves:
- Enhanced perinatal care and timely management of high-risk pregnancies.
- Improved fetal monitoring to reduce the risk of in utero hypoxia.
- Widespread training in the ABCDE resuscitation technique for obstetricians, pediatricians, and anesthesiologists.
- Proper resuscitation equipment in all hospital delivery rooms.
- Presence of personnel skilled in neonatal resuscitation for every delivery.