A neonate (newborn) refers to an infant during the first 28 days of life, starting from the clamping of the umbilical cord. Neonatology is the branch of medicine that studies neonatal physiology, pathology, disease prevention, and care. Originally part of pediatrics, neonatology has developed rapidly in recent decades and is now an independent scientific discipline. Neonates are the continuation of fetal life and are closely related to obstetrics. Thus, neonatology is also considered a part of perinatology.
Perinatology is a medical field that focuses on factors influencing the health of fetuses and neonates during the perinatal period. It involves obstetrics, neonatology, and associated disciplines such as genetics, biochemistry, immunology, and biomedical engineering. As an interdisciplinary field, perinatology plays a crucial role in improving population quality and reducing perinatal mortality rates. The perinatal period, also known as the perinatal stage, refers to a specific timeframe surrounding birth. International definitions of this period vary:
- From 28 weeks of gestation (when fetal weight is approximately 1,000 g) to the first seven days postpartum.
- From 20 weeks of gestation (when fetal weight is approximately 500 g) to 28 days postpartum.
- From 28 weeks of gestation to 28 days postpartum.
The World Health Organization (WHO) and the International Classification of Diseases (ICD-11) define the perinatal period as spanning from 22 weeks of gestation to seven days postpartum. Infants during this period are referred to as perinatal infants. This transitional phase from the intrauterine to extrauterine environment marks the highest mortality and morbidity rates during a human's life, particularly within the first 24 hours postpartum.
Classification of Neonates
Neonates can be categorized using several different methods. Common clinical classifications include gestational age, birth weight, the relationship between birth weight and gestational age, and postnatal age.
Classification by Gestational Age
Gestational age (GA) refers to the time from the first day of the last normal menstrual period to delivery, expressed in weeks. Based on gestational age, neonates can be classified as term infants, preterm infants, or post-term infants:
- Term infants: Neonates whose gestational age ranges between 37 weeks and less than 42 weeks (259–293 days).
- Preterm infants: Neonates whose gestational age is less than 37 weeks (<259 days). These include:
- Extremely preterm infants: Gestational age <28 weeks.
- Very preterm infants: Gestational age 28–32 weeks.
- Moderately preterm infants: Gestational age 32–34 weeks.
- Late preterm infants: Gestational age between 34 weeks and less than 37 weeks (238–258 days).
- Post-term infants: Neonates whose gestational age is 42 weeks or more (≥294 days).
Classification by Birth Weight
Birth weight (BW) refers to the neonate's weight measured within one hour after birth. Neonates can be categorized as normal birth weight (NBW) infants, low birth weight (LBW) infants, or macrosomic infants:
- Normal birth weight infants: Neonates with a birth weight of 2,500–4,000 g.
- Low birth weight infants: Neonates with a birth weight of less than 2,500 g. Among these:
- Very low birth weight infants (VLBW): Birth weight <1,500 g.
- Extremely low birth weight infants (ELBW): Birth weight <1,000 g.
- Macrosomic infants: Neonates with a birth weight greater than 4,000 g.
Most LBW infants are preterm, although some may be full-term or post-term and small-for-gestational-age.
Classification by Relationship Between Birth Weight and Gestational Age
Based on birth weight relative to gestational age, neonates can be divided into appropriate-for-gestational-age infants (AGA), small-for-gestational-age infants (SGA), and large-for-gestational-age infants (LGA):
- AGA infants: Birth weight falls between the 10th and 90th percentiles relative to gestational age.
- SGA infants: Birth weight is below the 10th percentile for gestational age.
- LGA infants: Birth weight is above the 90th percentile for gestational age.
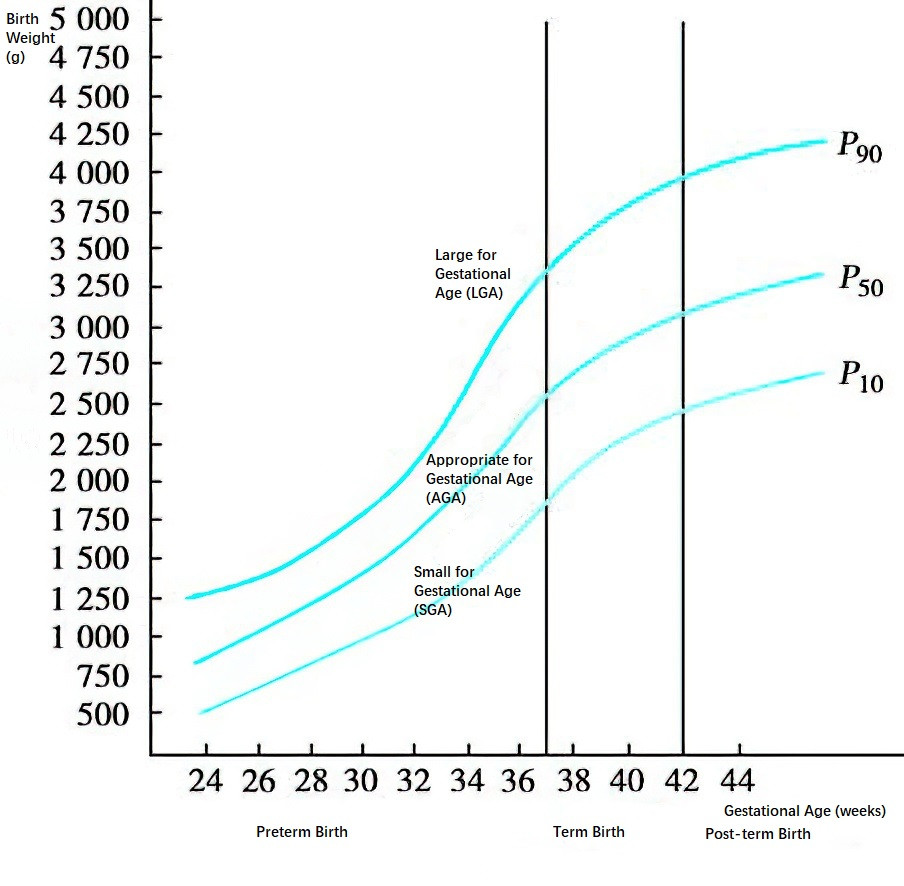
Figure 1 Percentile curves of gestational age and birth weight for neonates
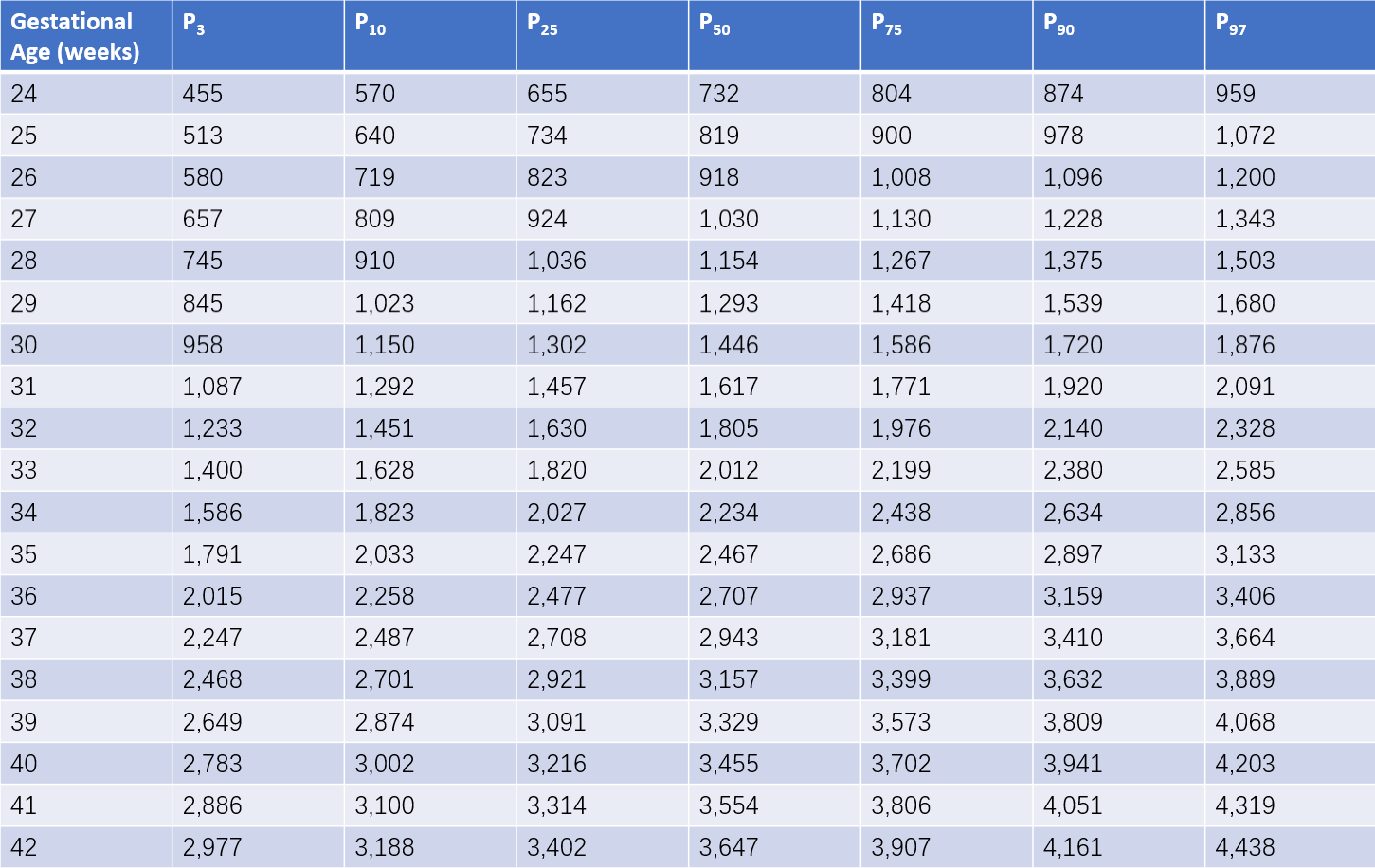
Table 1 Reference percentiles for birth weight of male neonates at different gestational ages (Unit: g)
Note: P represents percentiles.
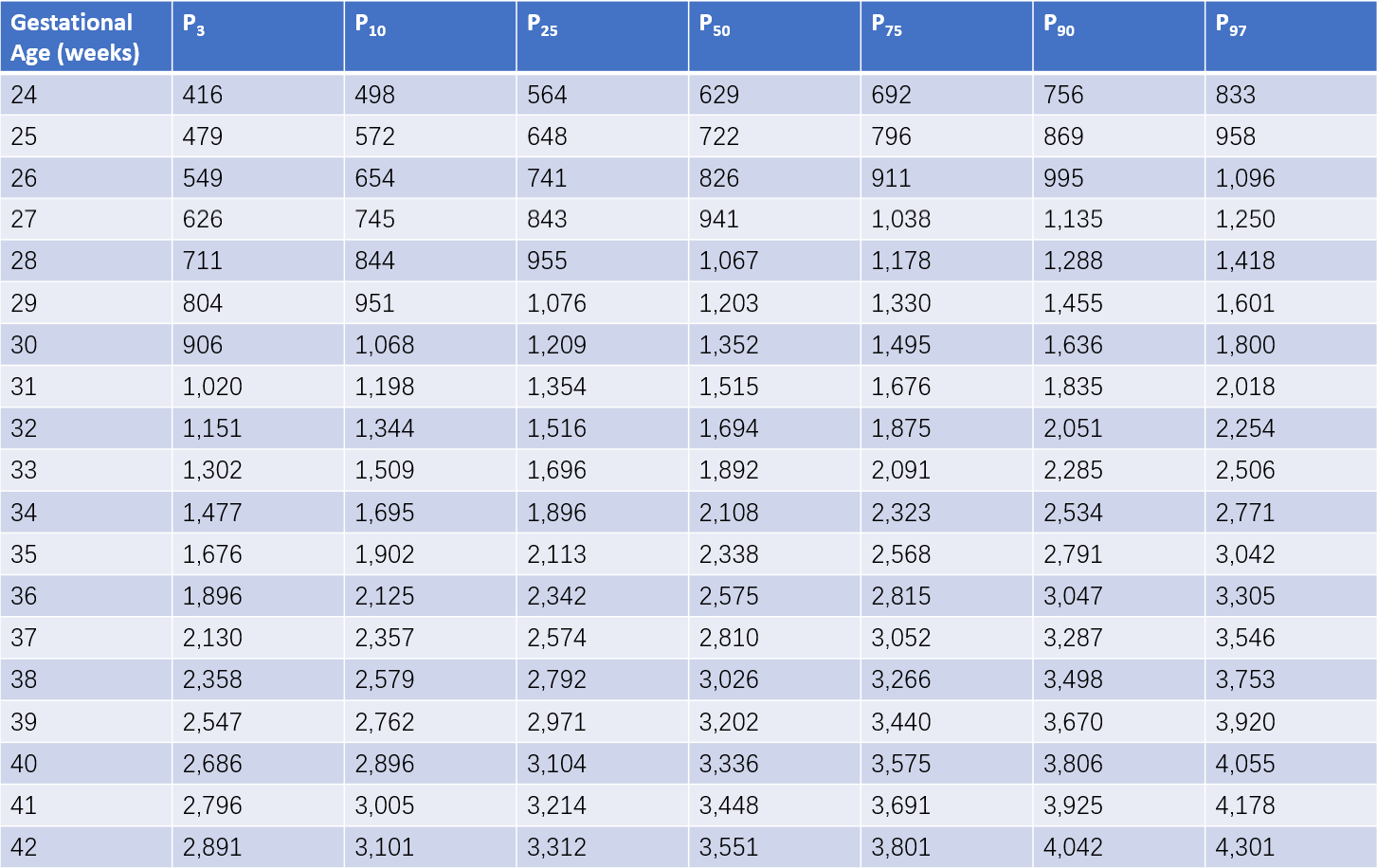
Table 2 Reference percentiles for birth weight of female neonates at different gestational ages (Unit: g)
Note: P represents percentiles.
Classification by Postnatal Age
Neonates can be categorized as early newborns or late newborns:
- Early newborns: Neonates within the first week of life. They are also considered perinatal infants, with the highest morbidity and mortality rates in the entire neonatal period, necessitating heightened care and monitoring.
- Late newborns: Neonates in the second to fourth weeks of life.
High-Risk Infants
High-risk infants are neonates who have experienced or are predisposed to critical illnesses requiring intensive monitoring. Factors often associated with high-risk neonates include:
- Maternal medical history: Conditions such as diabetes, infections, chronic cardiovascular or pulmonary diseases, smoking, substance abuse, excessive alcohol consumption, Rh-negative blood type, stillbirth history, or sexually transmitted infections.
- Maternal pregnancy history: Factors such as maternal age over 40 or under 16, vaginal bleeding, pregnancy-induced hypertension, preeclampsia or eclampsia, premature rupture of membranes, placental abruption, or placenta previa.
- Delivery history: Complicated deliveries, surgical deliveries, precipitous labor, prolonged labor, or administration of sedatives or analgesics during delivery.
- Neonatal factors: Conditions such as asphyxia, multiple births, preterm birth, small-for-gestational-age status, macrosomia, intrauterine infections, genetic metabolic disorders, or congenital anomalies.
Levels of Neonatal Care Units
Classification of Neonatal Care Units by Medical Care and Equipment Levels
Neonatal care units are categorized into four levels based on medical care quality and equipment requirements:
- Level I Nursery: This is a standard infant care room designed for healthy neonates. Its primary purpose involves teaching parents caregiving skills and methods as well as screening for common hereditary and metabolic disorders. Rooming-in arrangements for mothers and infants are encouraged to facilitate breastfeeding, strengthen maternal-infant bonding, and promote physical and psychological well-being for the newborn.
- Level II Nursery: This is a general neonatal care unit suitable for preterm infants with gestational age greater than 32 weeks and birth weight ≥1,500 g (≥1,200 g in developed countries). It also accommodates sick infants who do not require circulatory or respiratory support and monitoring.
- Level III Nursery (Neonatal Intensive Care Unit, NICU): This is a specialized unit for critically ill neonates, including preterm infants with birth weight <1,500 g or gestational age <32 weeks. It also admits severe cases transferred from Level I or Level II nurseries. NICU must be equipped with highly trained personnel specialized in neonatal emergency care and advanced neonatal transport systems. Typically, NICUs are located in teaching hospitals affiliated with medical schools or in large children's hospitals.
- Level IV Nursery (Level III Plus): This refers to teaching hospitals with capabilities for complex surgical procedures, such as those required for congenital heart defects. These facilities are equipped with subspecialties in pediatric internal medicine, pediatric surgery, pediatric anesthesiology, and others. They are capable of neonatal transport and often serve as centers for continuing medical education and expertise dissemination.
Admission Criteria for NICU
NICU accommodates the following cases:
- Neonates receiving assisted ventilation or within 24 hours following extubation.
- Neonates with severe perinatal asphyxia.
- Neonates with severe cardiopulmonary diseases, hyperbilirubinemia, cold injuries, or respiratory apnea.
- Neonates within 24 hours post-major surgery, especially within the critical postoperative period.
- Preterm infants with birth weight <1,500 g.
- Neonates requiring total parenteral nutrition or exchange transfusion.
- Neonates experiencing refractory seizures.
- Neonates suffering from multi-organ failure, including conditions such as shock, disseminated intravascular coagulation (DIC), heart failure, or kidney failure.
Monitoring Equipment and Alarm Systems in NICU
NICUs are equipped with monitoring devices and alarm systems for continuous monitoring of vital signs:
- Cardiac Monitoring: Tracks heart rate, rhythm, and changes in electrocardiographic waveforms.
- Respiratory Monitoring: Monitors respiratory rate, rhythm, and apnea episodes.
- Blood Pressure Monitoring: Includes both invasive (direct) and non-invasive (indirect) methods.
- Direct method (invasive): Involves inserting a catheter into an artery (commonly the umbilical artery) for continuous blood pressure measurement. This method provides accurate readings but is technically complex, associated with complications, and typically reserved for cases with poor peripheral perfusion.
- Indirect method (non-invasive): Involves placing a cuff around the upper arm to intermittently measure and automatically display systolic, diastolic, and mean arterial pressures. Although less accurate than the direct method, it is simpler, has no associated complications, and is the most commonly used method for blood pressure monitoring in NICUs.
- Temperature Monitoring: Neonates are placed on a radiant warmer or in an incubator, and a temperature monitor sensor is attached to the abdominal wall skin for continuous temperature display.
- Blood Gas Monitoring: Includes devices for monitoring transcutaneous oxygen tension (TcPO2), transcutaneous carbon dioxide tension (TcPCO2), and transcutaneous oxygen saturation (TcSO2). These devices offer non-invasive, continuous, and automatic monitoring, allowing observation of trends in blood gas changes. However, their measurements may deviate from arterial blood gas values, particularly in neonates with poor peripheral circulation, making them less accurate in such cases. Periodic arterial blood gas testing remains necessary. Transcutaneous oxygen saturation (TcSO2) is relatively accurate and is currently a commonly used method for dynamic monitoring of blood oxygen levels in NICUs.