Vitamin A deficiency (VAD) refers to any form and degree of vitamin A insufficiency within the body, including clinical, subclinical, and borderline subclinical (or marginal) vitamin A deficiency. Clinical vitamin A deficiency manifests as classic signs such as hyperkeratosis and xerophthalmia. Subclinical and borderline subclinical vitamin A deficiency, on the other hand, do not present with specific symptoms but are often associated with broader effects such as recurrent respiratory infections, diarrhea, and anemia, which increase illness incidence and mortality in infants and young children.
Vitamin A deficiency is one of the most widespread public health nutrition issues globally. Approximately 127 million preschool-aged children are vitamin A deficient, with 4.4 million suffering from some degree of xerophthalmia. In developing countries, 7.2 million pregnant women are vitamin A deficient, and 13.5 million are classified as marginally deficient. Annually, over 6 million pregnant women experience night blindness linked to vitamin A deficiency.
Absorption and Metabolism
Sources of Vitamin A
Vitamin A refers to a group of retinoid compounds with all-trans retinol biological activity, including retinol, retinal, retinyl esters, and retinoic acid. Retinoic acid is the most important active form of vitamin A in the body, mediating various physiological functions. Vitamin A can be derived from two main sources. One source is animal-based foods containing retinyl esters, such as milk, eggs, and animal liver, which are rich in vitamin A. The other source is plant-based foods containing provitamin A carotenoids, particularly beta-carotene, which has the highest vitamin A activity and is abundant in dark-colored vegetables and fruits. Both vitamin A and beta-carotene are fat-soluble, and their digestion and absorption mechanisms are similar to those of lipids.
Transport of Vitamin A
Vitamin A is absorbed by intestinal cells, combined with chylomicrons, and transported through the lymphatic system into the bloodstream, eventually reaching the liver. In the liver, it is esterified into retinyl esters and stored in stellate cells. When peripheral target tissues require it, liver-stored retinyl esters are hydrolyzed by esterases into retinol, which binds to retinol-binding protein (RBP) synthesized by the liver. This retinol-RBP complex then binds to transthyretin in plasma to form a transport complex that reduces renal filtration of retinol and delivers it to target cells.
Nuclear Receptors for Vitamin A
The aforementioned complex binds to RBP receptors on target cells, releasing retinol into the cells, where it is converted into retinoic acid. Retinoic acid binds to specific nuclear receptors, such as retinoic acid receptors (RAR) and retinoid X receptors (RXR), to regulate the expression of hundreds of genes. Through this role as a nuclear hormone, retinoic acid exerts its physiological functions.
Physiological Functions and Pathological Changes
Formation of Photosensitive Substances in Vision Cells
The eyes are particularly sensitive to vitamin A deficiency. In retinal rod cells, 11-cis-retinal combines with opsin to form rhodopsin, which is necessary for dim-light vision. When light strikes the retina, it triggers a series of complex biochemical reactions, generating nerve impulses. During this process, some retinal is converted to retinol and excreted, requiring continuous vitamin A replenishment to maintain normal vision.
Influence on Epithelial Stability and Integrity
Vitamin A deficiency causes mucus-secreting cells in epithelial tissues to be replaced by keratin-producing cells. This change leads to dryness of the skin, conjunctiva, and cornea, and in severe cases, xerophthalmia and corneal ulcers. The early pathological change in epithelial tissue is dryness, followed by excessive keratinization and reduced gland secretion. These changes affect epithelial tissues throughout the body, particularly in the respiratory, digestive, and urinary tracts.
Promotion of Growth and Maintenance of Reproductive Functions
Vitamin A influences growth and development by affecting RNA and DNA synthesis and growth hormone secretion. It also impacts normal sperm production and placental development.
Maintenance and Enhancement of Immune Function
Vitamin A plays a role in maintaining immune activity by supporting the lymphocyte pool, participating in T-cell-mediated immune responses, and enhancing the ability of immune cells to produce antibodies. It promotes the production of certain cytokines by T lymphocytes, and deficiency in vitamin A impairs these immune functions.
Influence on Hematopoiesis
Vitamin A deficiency affects the transport and storage of iron, potentially leading to anemia.
Etiology
Insufficient Dietary Intake
Vitamin A deficiency occurs at a much higher rate in children under five compared to adults. This is primarily because vitamin A and carotenoids are not easily transported across the placenta to the fetus. Consequently, newborns have significantly lower serum and liver vitamin A levels compared to their mothers. If insufficient vitamin A is consumed postnatally, deficiencies can easily arise.
Impaired Digestion and Absorption
As a fat-soluble vitamin, the digestion and absorption of vitamin A and carotenoids in the small intestine depend on bile salts. The dietary fat content is closely related to their absorption. A low dietary fat intake, reduced secretion of pancreatic enzymes and bile (due to conditions such as pancreatitis or gallstones), and gastrointestinal dysfunction may all impair digestion and absorption of vitamin A and carotenoids.
Impaired Storage and Utilization
Any condition that affects liver function can reduce the body’s storage of vitamin A, resulting in deficiency. Additionally, conditions associated with high metabolic demand, such as infectious diseases, can deplete vitamin A reserves, particularly in children. Measles, scarlet fever, and tuberculosis are examples of diseases that can increase vitamin A consumption and contribute to the development of vitamin A deficiency.
Clinical Manifestations
The clinical manifestations of vitamin A deficiency are closely related to the stage and severity of the deficiency. In subclinical and borderline subclinical cases, symptoms are nonspecific and primarily include increased susceptibility to infections and anemia. Only in cases of severe deficiency does the classical symptom of vitamin A deficiency, xerophthalmia, become apparent.
Ocular Manifestations
The earliest recognized symptoms and signs of vitamin A deficiency are ocular. Night blindness or difficulty seeing in dim light develops first. After several weeks, xerophthalmia begins to appear, characterized by dryness and loss of luster in the conjunctiva and cornea, along with itching and reduced tear production. An eye examination may reveal wrinkled, dry folds near the corneal margins and keratinized epithelial accumulations forming foamy white spots, referred to as conjunctival xerosis or Bitot's spots. As the condition progresses, the cornea becomes dry, cloudy, and softened, accompanied by photophobia and eye pain. Rubbing of the eyes, often due to discomfort, can lead to infection. Severe cases may result in corneal ulceration, necrosis, perforation, prolapse of the iris and lens, and eventual blindness.
Skin Manifestations
Early skin symptoms include dryness, flaking, and itching. Over time, epithelial thickening and keratinization develop, with reduced sweat production. Keratinized material may fill hair follicles, resulting in follicular papules. The skin feels rough, resembling fine sandpaper, especially on the extensor surfaces of the limbs, shoulders, and, in some cases, the neck, back, or even the face. Follicular keratinization leads to dry, dull, and fragile hair that is prone to shedding. Nails, including those of fingers and toes, may become brittle, fragmented, and ridged.
Growth and Development Disorders
Severe deficiency can impair growth, leading to delayed height development, worn tooth enamel, loss of luster, and increased risk of dental caries.
Increased Susceptibility to Infection
During subclinical or borderline subclinical stages, immune function is compromised, resulting in recurrent respiratory and gastrointestinal infections. These infections often become chronic, increasing disease prevalence and mortality, particularly among children aged 6 months to 2 years.
Anemia
Vitamin A deficiency can lead to increased iron storage in the liver, reduced plasma iron levels, and microcytic, hypochromic anemia resembling iron-deficiency anemia.
Diagnosis
Clinical Diagnosis
A clinical diagnosis is based on a history of insufficient intake or increased consumption, along with evident clinical manifestations associated with vitamin A deficiency. Laboratory tests revealing low serum vitamin A levels can assist in confirming the diagnosis and monitoring treatment effectiveness. Subclinical and borderline subclinical cases, which lack specific clinical symptoms, rely on laboratory tests and epidemiological data for diagnosis.
Laboratory Diagnosis
Plasma Retinol
Retinol is the primary form of serum vitamin A and serves as a key indicator for diagnosing vitamin A deficiency. Serum vitamin A levels below 0.7 μmol/L indicate vitamin A deficiency. Severe deficiency is diagnosed when serum vitamin A falls below 0.35 μmol/L and is accompanied by xerophthalmia. If xerophthalmia symptoms are absent, the case is classified as subclinical deficiency. Serum vitamin A levels between 0.7 and 1.05 μmol/L suggest borderline subclinical vitamin A deficiency.
Relative Dose Response (RDR)
RDR provides an indirect estimate of liver vitamin A reserves. Subjects receive an oral dose of retinol (450 μg), and plasma retinol concentrations are measured before administration (A0) and 5 hours after (A5). The RDR value is calculated using the formula:
RDR (%) = (A5 - A0) / A5 × 100%.
An RDR value greater than 20% indicates subclinical vitamin A deficiency.
Plasma Retinol-Binding Protein (RBP) Testing
RBP levels correlate with serum vitamin A levels. Values below 23.1 mg/L suggest potential vitamin A deficiency. However, RBP levels may decrease in cases of infection or protein-energy malnutrition, necessitating additional testing, such as for C-reactive protein.
Urine Exfoliated Cell Analysis
Adding 1% methylene violet to fresh midstream urine and counting epithelial cells can aid in diagnosis. In the absence of urinary tract infections, more than three epithelial cells per mm3 is abnormal. Identifying keratinized epithelial cells has diagnostic significance.
Dark Adaptation Testing
Dark adaptation meters and retinal electrocurrent tests can detect visual abnormalities in dim light, supporting diagnostic assessments.
Treatment
Even subclinical vitamin A deficiency requires early supplementation to prevent progression.
Dietary Adjustment and Addressing Underlying Causes
Providing animal-based foods rich in vitamin A or plant-based foods high in carotenoids, such as dark-colored vegetables, can help manage the deficiency. Fortified foods, such as infant formula and complementary foods containing vitamin A, are useful in areas where resources allow. Addressing any underlying conditions contributing to the deficiency is also essential.
Vitamin A Supplementation
In 2005, WHO, UNICEF, and the International Vitamin A Consultative Group (IVACG) collaborated on the Innocenti Micronutrient Research Report to establish guidelines for treating vitamin A deficiency. These guidelines recommend the use of vitamin A formulations for supplementation in individuals affected by deficiency.
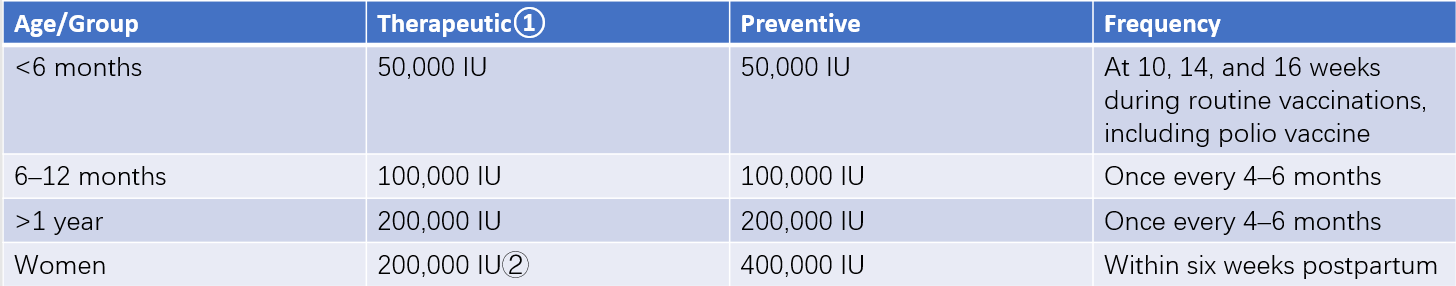
Table 1: Routine and age-appropriate recommendations for preventive and therapeutic high-dose vitamin A supplementation
Notes:
① For individuals of the respective age groups, those diagnosed with xerophthalmia are to receive an immediate single dose, a second dose after 24 hours, and a third dose after two weeks. For patients diagnosed with measles, an immediate single dose is administered, followed by a second dose after 24 hours. For those diagnosed with protein-energy malnutrition, an initial single dose is administered, followed by daily maintenance-level supplementation.
② Women of childbearing age (13–49 years) diagnosed with active corneal damage are to receive 200,000 IU of vitamin A immediately, a second dose after 24 hours, and a third dose after two weeks. Women with mild ocular signs (such as night blindness and/or Bitot's spots) are recommended to supplement 10,000 IU/day or 25,000 IU/week of vitamin A for no less than three months.