Nutrients and Dietary Reference Intake (DRI)
Nutrition refers to the biological process through which the human body obtains and utilizes food to sustain life activities. Substances in food that can sustain life through digestion, absorption, and metabolism are called nutrients. There are more than 40 essential nutrients for human life, which can be grouped into six categories based on their structure and function: proteins, lipids, carbohydrates, minerals, vitamins, and water. Among these, the first three categories are energy-providing nutrients. The energy contribution of proteins, lipids, and carbohydrates in meeting human energy needs is approximately in the ratio of 1:3:6 (proteins: 8%–15%; lipids: 20%–48%; carbohydrates: 50%–65%). When oxidized in the body, each gram of protein, fat, and carbohydrate produces an average of 4 kcal, 9 kcal, and 4 kcal of energy, respectively (Note: energy is measured in kilocalories [kcal] or kilojoules [kJ], where 1 kcal ≈ 4.184 kJ). Although non-energy nutrients (minerals, vitamins, and water) do not contribute to energy, they are crucial for maintaining normal physiological functions and metabolism. Nutrients are further categorized as macronutrients and micronutrients based on the amount needed by the body. Macronutrients include proteins, lipids, and carbohydrates, while micronutrients include minerals and vitamins.
The Dietary Reference Intake (DRI) system is composed of four key parameters:
- Estimated Average Requirement (EAR): This represents the average daily nutrient intake level estimated to meet the requirement of 50% of healthy individuals in a particular group based on gender, age, and physiological condition. EAR serves as the basis for establishing RNI.
- Recommended Nutrient Intake (RNI): This is the daily nutrient intake level estimated to meet the requirements of nearly all (97%–98%) healthy individuals in a specific group.
- Adequate Intake (AI): When insufficient research data prevents the calculation of EAR and RNI, AI is determined by observing or experimentally assessing the average daily nutrient intake of healthy individuals. Both AI and RNI can be used as target values for individual nutrient intake, although AI is less precise than RNI.
- Tolerable Upper Intake Level (UL): This refers to the safe upper limit for daily nutrient intake.
An intake exceeding UL increases the risk of adverse effects or toxicity.
Energy Metabolism in Children
Energy is fundamental for maintaining life-sustaining activities and supporting growth and development. The optimal state of energy metabolism is a balance between energy intake and expenditure, as both energy deficiency and excess can have negative effects on health. The total energy expenditure in children consists of five components: basal metabolism, thermic effect of food, energy used for growth, physical activity, and excreta-related losses.
Basal Metabolism (BM)
Basal metabolism refers to the minimal energy expenditure required to sustain essential life functions. Basal Metabolic Rate (BMR) is an indicator that reflects basal metabolism. In children, the energy required for basal metabolism is higher than in adults but decreases with age. For infants, BMR is approximately 55 kcal/(kg·d), decreasing to 44 kcal/(kg·d) at 7 years of age, and about 30 kcal/(kg·d) by 12 years of age. In adults, BMR ranges between 25–30 kcal/(kg·d).
Thermic Effect of Food (TEF)
The process of digesting, absorbing, and metabolizing food consumes energy, which is referred to as the thermic effect of food or the specific dynamic action of food. TEF varies with the composition of the food: carbohydrates contribute 6% of their energy as the thermic effect, fats contribute 4%, and proteins contribute 30%. Since infant diets contain a higher proportion of protein, TEF accounts for 7%–8% of their total energy expenditure. For older children, whose diets are typically composed of mixed foods, TEF accounts for 5% of the total energy expenditure.
Energy for Growth
Energy is consumed during the synthesis required for tissue growth, which is unique to children. The energy required for growth is proportional to the growth rate of children and decreases with age.
Energy for Physical Activity
Energy expenditure due to activity depends on body size, activity intensity and duration, and the type of activity. The energy required for physical activity varies significantly among individuals and increases with age. When energy intake is inadequate, children may exhibit reduced physical activity.
Energy Loss through Excreta
In normal conditions, the loss of energy from undigested and unabsorbed food accounts for approximately 10% of total energy. During diarrhea, this loss increases.
Typically, basal metabolism accounts for 50% of total energy expenditure, the thermic effect of food accounts for 7%–8%, energy for growth and physical activity accounts for 32%–35%, and energy loss through excreta accounts for 10%. The average energy requirement for infants aged ≤6 months is 90 kcal/(kg·d), while for those aged 7–12 months, it is 80 kcal/(kg·d).
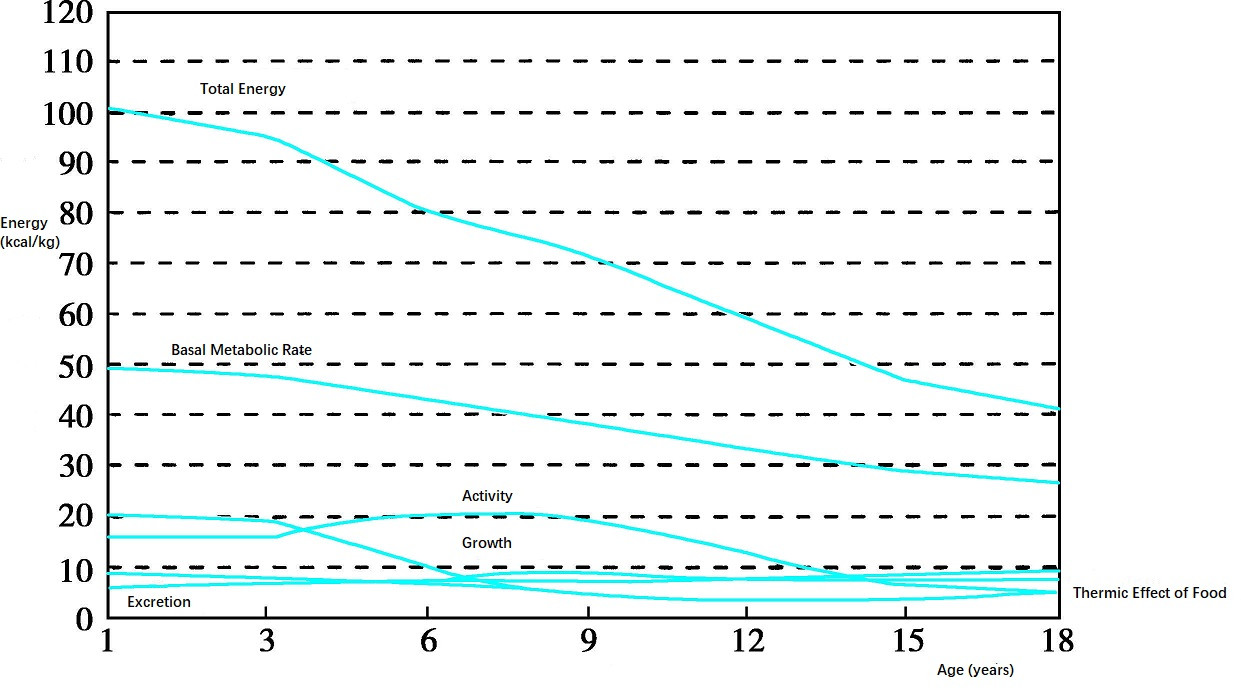
Figure 1 Relationship between energy distribution and age
Energy-Providing Nutrients
Proteins
Proteins are essential components of cells, tissues, and organs, with their primary role being the construction of body tissues and the regulation of physiological functions. Their secondary role is energy production, accounting for 8%–15% of total energy. The recommended nutrient intake (RNI) of protein for infants under one year of age is 1.5–3 g/(kg·d). The building blocks of proteins are amino acids. Of the 21 amino acids that constitute human proteins, nine cannot be synthesized by the body (or are synthesized too slowly to meet the body's needs) and must be obtained from food. These are called essential amino acids, including leucine, isoleucine, valine, threonine, methionine, phenylalanine, tryptophan, lysine, and histidine, with histidine being an essential amino acid specifically for infants.
Some amino acids become necessary under certain pathological conditions, where the body cannot synthesize them in sufficient amounts, or they reduce the body's demand for essential amino acids. These are referred to as conditional essential or semi-essential amino acids. Proteins that contain a complete spectrum of essential amino acids, are similar in composition to human proteins, and offer high nutritional value are termed high-quality proteins. These are primarily derived from animal sources and soy protein. Due to the rapid growth of infants and young children, ensuring a supply of high-quality protein is particularly important; high-quality protein intake should account for more than 50% of total protein consumption.
The mutual supplementation of essential amino acids between different foods, known as the protein complementary action, can improve the biological value of food. This is achieved through the rational combination and processing of foods.
Lipids
Lipids include fats (triglycerides) and lipoids, which encompass phospholipids, sterols, glycolipids, and lipoproteins. The primary function of fat is energy storage and energy production, making it the second energy-providing nutrient in the body. The proportion of energy derived from fat decreases with age, from about 48% at birth to 20%–30% in older children. Fats also play key roles as structural components of cells and in functions such as insulation, lubrication, and endocrine regulation.
The basic units of fats are fatty acids, which can be categorized based on the number of carbon atoms into short-chain (<6 carbons), medium-chain (8–12 carbons), and long-chain (14–24 carbons) fatty acids. Some very-long-chain fatty acids are present in the brain and other specific tissues. Fatty acids can also be grouped into saturated and unsaturated fatty acids, depending on the presence of double bonds. Saturated fatty acids are often solid at room temperature, while unsaturated fatty acids are typically liquid.
Fatty acids that are indispensable but cannot be synthesized by the body are called essential fatty acids, such as linoleic acid and alpha-linolenic acid. Linoleic acid is the most essential fatty acid for maintaining health and can be converted in the body into linolenic acid and arachidonic acid (AA). Alpha-linolenic acid can be further metabolized into polyunsaturated fatty acids, including eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Essential fatty acids and their derivatives have crucial physiological functions, such as participating in phospholipid synthesis to maintain cell membrane structure and function, regulating cholesterol metabolism to prevent atherosclerotic plaque formation, and supporting visual function and brain development through the action of EPA and DHA.
Fat sources include edible oils, which are nearly 100% fat, as well as fat-rich foods like animal products and nuts. Linoleic acid is predominantly found in vegetable oils and nuts (e.g., walnuts and peanuts), while alpha-linolenic acid is present in fish oil and nuts. To ensure adequate essential fatty acid intake for infants, oils rich in linoleic acid and alpha-linolenic acid are recommended. Breast milk is also a rich source of essential fatty acids. Energy from essential fatty acids should account for 1%–3% of the total energy provided by fats.
Carbohydrates
Carbohydrates are the primary source of energy, contributing 50%–65% of total energy intake. They also serve as components of body tissues and vital biological molecules, while playing roles in preventing ketosis and sparing proteins. All carbohydrates are ultimately broken down into glucose for absorption and utilization by the body. Oxidation of glucose produces energy, while unused glucose can be stored as glycogen or converted to fat. Non-sugar compounds such as lactate, glycerol, and glucogenic amino acids can also be converted into glucose or glycogen through a process known as gluconeogenesis.
Sources of carbohydrates include cereals, fruits, root and tuber vegetables, and legumes. The ability of carbohydrate-containing foods to raise blood glucose is quantified as the glycemic index (GI). The GI of foods is influenced by the type of carbohydrate and its processing method. Foods with a GI >70 are classified as high-GI foods, those with a GI of 55–70 are medium-GI foods, and those with a GI <55 are low-GI foods. The GI is widely applied in dietary management for individuals with diabetes or obesity.
Dietary fiber, a type of carbohydrate that cannot be digested or absorbed by the human body, provides numerous health benefits. It includes non-starch polysaccharides (e.g., cellulose, hemicellulose, pectin, and beta-glucan), resistant oligosaccharides (e.g., fructooligosaccharides), resistant starch, and lignin. Dietary fiber functions to increase satiety, promote gut health, stimulate the growth of probiotics, and facilitate bowel movements. In infants, dietary fiber mainly comes from partially digested lactose, oligosaccharides in milk, and undigested starch in food. In older children, dietary fiber sources include grains, legumes, vegetables, fruits, and potatoes.
To support the growth and development of children, energy supply should be prioritized, followed by adequate protein intake. Notably, the central nervous system primarily relies on glucose for energy. A lack of carbohydrates during infancy may affect brain cell growth and development, increasing the risk of hypoglycemia.
Non-Energy-Producing Nutrients
Minerals
Among the elements that constitute the human body, those other than carbon, hydrogen, oxygen, and nitrogen found in organic compounds are categorized as minerals. Based on their concentration in the body, minerals are divided into macrominerals and trace elements. Minerals accounting for more than 0.01% of body weight are classified as macrominerals, which include calcium, magnesium, potassium, sodium, phosphorus, sulfur, and chlorine. Minerals with concentrations below 0.01% of body weight are referred to as trace elements. Minerals cannot be synthesized in the body and need to be obtained from food and water, though excessive intake of certain minerals can lead to toxicity. Minerals such as calcium, iron, zinc, and iodine are prone to deficiencies during infancy and childhood.
Macrominerals
Calcium and phosphorus together make up about 6% of the body's total weight, forming tissues such as bones and teeth. During infancy, calcium deposition is higher than at other stages of life. Calcium deficiency can hinder the development of bones and teeth in infants and young children, but excessive calcium intake may pose risks. Dairy products are typically the best sources of calcium due to their rich content and high bioavailability. It is recommended calcium intake as follows: For infants aged 0–6 months, adequate intake (AI) is 200 mg/day; for infants aged 6–12 months, AI is 250 mg/day. For toddlers aged 1 year and older, recommended nutrient intake (RNI) is 600 mg/day, gradually increasing to 1,000 mg/day as children grow.
Trace Elements
Essential trace elements include iron, iodine, zinc, selenium, copper, chromium, manganese, molybdenum, and cobalt, with more essential trace elements likely to be identified as research progresses.
Vitamins
Vitamins are a class of organic compounds essential for maintaining normal physiological functions in the human body. Despite their minimal concentrations, vitamins play vital roles in growth, development, and metabolism. Vitamins are divided into two categories: fat-soluble vitamins and water-soluble vitamins.
Fat-Soluble Vitamins
This group includes vitamins A, D, E, and K, most of which are stored in fat tissues and the liver. They are not easily excreted and may accumulate to toxic levels with excessive intake.
Water-Soluble Vitamins
These include the B-vitamin complex (e.g., vitamins B1, B2, B6, niacin, folic acid, vitamin B12, pantothenic acid) and vitamin C. Water-soluble vitamins are only stored in small amounts in the body, and deficiencies can quickly lead to noticeable symptoms.
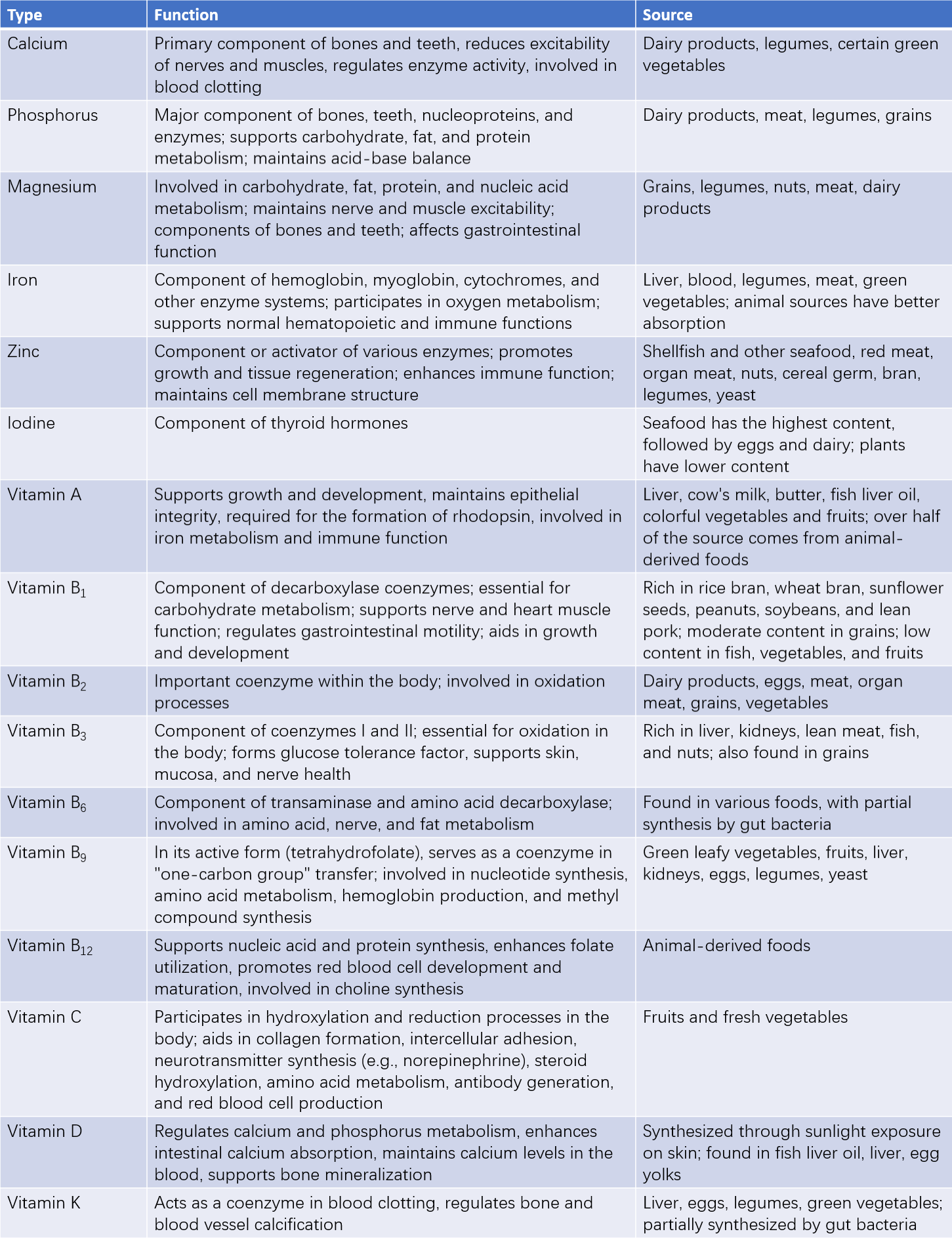
Table 1 Functions and sources of common minerals and vitamins
Water
Water is the most fundamental substance for sustaining life and is a crucial component of tissue cells. It regulates body temperature, participates in metabolism, maintains osmotic pressure in bodily fluids, and serves as a lubricant for various processes. In addition, water acts as a carrier in the metabolism of nutrients. Sources of water within the body include drinking water, water derived from food, and endogenous water generated through metabolism.
The water requirements of children depend on several factors, including energy intake, food composition, kidney maturation, and age. Infants, due to their high metabolic rate, require relatively large amounts of water, ranging from 110–155 mL/(kg·d). Starting at age three, water requirements decrease by approximately 10–25 mL/(kg·d) every three years. Children older than 13 years have water requirements similar to adults, at around 50–60 mL/(kg·d).
Relationship Between Digestive System Development and Child Nutrition
Children, being in a stage of growth and development, are characterized by high nutritional needs coupled with immature digestive and absorption functions.
Maturity of Digestive Enzymes and Nutrient Digestion and Absorption
Proteins
Newborns generally exhibit good protein digestion capacity. Gastric pepsin, which coagulates milk, has low activity at birth but increases significantly by three months, reaching adult levels by 18 months. Trypsin activity increases within the first week after birth and reaches adult levels by one month. During the first few months, the high permeability of epithelial cells in the small intestine facilitates the absorption of immunoglobulins from breast milk, but it also increases the absorption of foreign proteins (e.g., cow’s milk protein and egg protein), toxins, microorganisms, and incompletely metabolized substances, potentially leading to allergies or intestinal infections. Protein intake amounts and types thus necessitate careful consideration for infants, especially newborns.
Lipids
Gastric lipase is relatively well-developed in newborns, while pancreatic lipase activity is almost undetectable until children reach 2–3 years of age. Lipase in breast milk partially compensates for this deficiency. The ability of infants to absorb lipids increases with age. Fat absorption rates range from 65%–75% for preterm infants (28–34 weeks) to 90% for full-term infants, reaching over 95% by six months of age.
Carbohydrates
The primary carbohydrate in the diets of infants aged 0–6 months is lactose, followed by sucrose and small amounts of starch. Lactase activity in the intestines is higher in infants than adults, ensuring efficient digestion of lactose. Conversely, pancreatic amylase development is incomplete, with its activity gradually increasing after three months and reaching adult levels by two years of age. Complementary foods containing starch are recommended after six months of age.
Development of Feeding Skills
Patterns of Food Acceptance
In addition to innate taste reflexes to sweetness, sourness, and bitterness, infants develop taste perception through learned experiences.
Extrusion Reflex
From birth to 3–4 months of age, infants display an extrusion reflex characterized by tongue-raising and forward-thrust movements in response to solid foods. This reflex acts as a protective mechanism, preventing solid food from entering the airway and causing choking. During the transition to new foods, attempts to introduce pureed foods with a spoon may require repeated efforts.
Chewing
While sucking and swallowing are innate physiological functions, the development of chewing requires timely physiological stimulation and learning. Introducing pureed foods during the transition period serves as an appropriate stimulus for chewing development. Well-developed chewing abilities positively influence speech development. The sensitive period for learning proper chewing behaviors typically occurs between 4 and 6 months of age.