Skeletal System
Skull
In addition to head circumference, the evaluation of skull growth and development can also be based on the closure of sutures, the size of the fontanelles, and the timing of their closure. Due to passage through the birth canal, the cranial sutures often overlap slightly at birth, but this overlap disappears shortly after birth. The posterior fontanelle is either very small or closed at birth, and it typically closes no later than 6–8 weeks of age. The size of the anterior fontanelle at birth varies greatly (1–4 cm), with an average size of 2.5 cm. At 2–3 months of age, as the overlapping of the cranial bones resolves, the anterior fontanelle becomes slightly larger than at birth, after which it gradually ossifies and reduces in size, closing completely by no later than 2 years of age. The size of the anterior fontanelle is determined by the length of the line drawn between the midpoints of opposite edges. Examining the anterior fontanelle holds significant importance in pediatric clinical practice. Microcephaly accompanied by a small or prematurely closed anterior fontanelle may indicate brain growth impairment, while delayed closure of the anterior fontanelle can suggest hypothyroidism. A tense or bulging anterior fontanelle may indicate increased intracranial pressure, whereas a sunken fontanelle might signify dehydration.
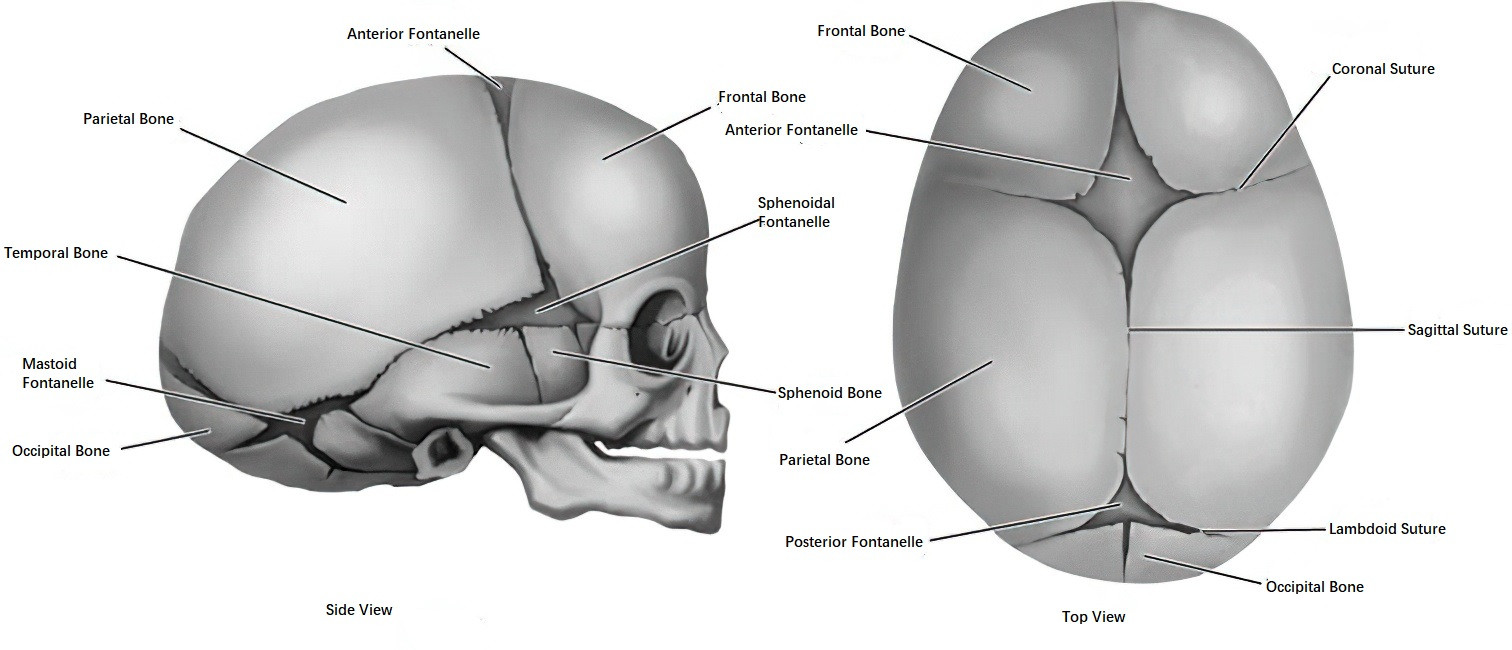
Figure 1 Development of the skull, anterior, and posterior fontanelles
Spine
Spinal growth reflects the development of the vertebrae. During the first year of life, the spine grows faster than the limbs; in later years, limb growth exceeds spinal growth. At birth, the spine shows no significant curvature and has a slight posterior convexity. By 3 months, the cervical spine begins to curve anteriorly as a result of head-raising activities. By 6 months, the ability to sit results in a posterior thoracic curve, and by 1 year of age, walking begins to produce an anterior lumbar curve. These natural spinal curvatures are stabilized by ligaments by approximately 6–7 years of age. Observing posture during sitting, standing, and walking, as well as choosing appropriate desks and chairs, plays an important role in maintaining normal spinal morphology in children.
Long Bones
The growth of long bones gradually progresses from the fetal period to adulthood. Long bone growth primarily occurs through the ossification of cartilage at the epiphyseal ends and subperiosteal bone formation, which leads to elongation and thickening. Growth ceases when the epiphyses fuse with the diaphysis.
With increasing age, the secondary ossification centers at the epiphyseal ends of long bones appear in a specific order and anatomical pattern. The appearance of these centers reflects the degree of long bone maturation. X-ray imaging is used to assess the timing, number, and morphological changes of ossification centers at different ages, and standardized measures of these findings are referred to as bone age.
At birth, no ossification centers are present in the wrist, but the distal femur and proximal tibia already show ossification. For early assessment of long bone growth, X-rays of the knee are taken in infants, whereas X-rays of the left hand and wrist are used in older children to examine wrist bones, metacarpals, and phalanges. The ossification centers of the carpal bones appear sequentially as follows: capitate and hamate (around 3 months), distal radial epiphysis (around 1 year), triquetrum (2–2.5 years), lunate (around 3 years), trapezium and trapezoid (3.5–5 years), scaphoid (5–6 years), distal ulnar epiphysis (6–7 years), and pisiform (9–10 years). By age 10, all 10 ossification centers are present, so the approximate number of carpal ossification centers between the ages of 1–9 corresponds to the age in years plus one. Evaluating bone age requires referencing standard radiographic atlases.
Bone growth is influenced by growth hormone (GH), thyroid hormones, and sex hormones. Bone age has important diagnostic value in clinical practice. For example, it is significantly delayed in conditions such as hypothyroidism and growth hormone deficiency, while it advances in cases of true precocious puberty or congenital adrenal hyperplasia. However, due to the wide variation in the normal age of ossification center appearance, caution is required when diagnosing delayed bone age.
Teeth
Tooth growth is related to bone development, but since their embryonic origins differ, their growth patterns are not entirely parallel. At birth, the primary teeth are already mineralized, with the tooth buds hidden within the jawbone and covered by the gums. The permanent teeth begin mineralizing in the neonatal period, and by 18–24 months, the third permanent molars have also begun ossification. Humans have two dentitions in their lifetime: primary teeth (20 total) and permanent teeth (28–32 total).
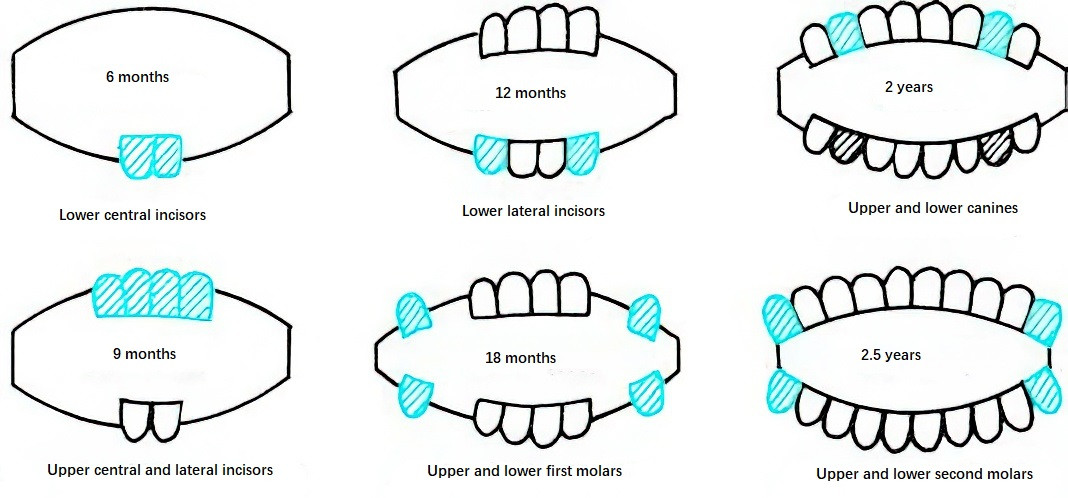
Figure 2 Sequence of primary tooth eruption
Primary teeth typically erupt between 4–10 months of age. Delayed eruption is defined as the absence of erupted teeth by 13 months of age. Generally, lower teeth erupt before upper teeth, and the sequence progresses from the front to the back, with most primary teeth fully erupted by age 3. Variations in the timing and sequence of eruption are influenced by genetics, hormones, and diet texture.
Around age 6, the first permanent tooth (usually the first permanent molar, also known as the "six-year molar") erupts behind the second primary molar. Between the ages of 6–12, primary teeth are gradually replaced by their corresponding permanent teeth. During this mixed dentition stage, the first and second premolars replace the first and second primary molars. By age 12, the second permanent molars erupt, and the third permanent molar (wisdom tooth) generally erupts after age 18, although some individuals never develop wisdom teeth. Because the first permanent molars erupt early and can be easily overlooked, attention to their care is particularly important.
Tooth eruption is a physiological process, though some children may experience mild symptoms such as low-grade fever, increased salivation, drooling, poor sleep, or irritability during eruption. Abnormal tooth development may occur in conditions such as ectodermal dysplasia, calcium or fluoride deficiency, and hypothyroidism.
Reproductive System
This can be seen in the section on endocrine conditions for detailed information.