Fetoscopy is a technique that involves the use of a 2–3 mm fiber-optic endoscope, introduced into the amniotic sac through a trochar needle via the maternal abdominal wall and the uterine wall, for the examination and in-utero treatment of the fetus. The primary applications of fetoscopy are as follows:
Fetoscopic Examination
Fetoscopy can be used for observing fetal external features (e.g., cleft lip, albinism) or obtaining fetal tissue biopsies for pathological analysis or genetic diagnosis. However, due to advancements in ultrasound and molecular genetic technologies, fetoscopic examinations for the sole purpose of sampling or visual inspection are no longer routine.
Fetoscopic Treatment
In-Utero Treatment of Twin-to-Twin Transfusion Syndrome (TTTS)
Twin-to-twin transfusion syndrome (TTTS) is a severe complication seen in 10–15% of monochorionic diamniotic twin pregnancies. Vascular anastomoses between placental vessels can manifest as arterial-arterial (A-A), venous-venous (V-V), or arteriovenous (A-V) connections. Typical TTTS involves unidirectional flow through deep A-V anastomoses within the placental villous lobules, lacking superficial bidirectional and protective A-A anastomoses. Without timely intervention, severe TTTS cases exhibit a mortality rate of 90–100%. Fetoscopic laser coagulation of placental anastomotic vessels (FLOC) is the most widely applied fetoscopy technique for treating TTTS, achieving a survival rate of at least one fetus in 80% of cases, and both twins in more than 50% of cases.
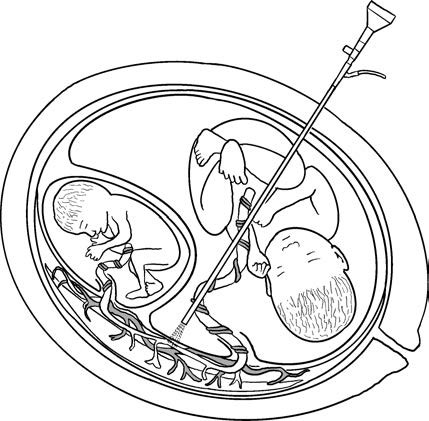
Figure 1 Fetoscopic laser ablation of placental anastomotic vessels for the treatment of twin-to-twin transfusion syndrome (TTTS)
Indications
These include Quintero stage II to IV TTTS cases as well as selected stage I cases. Approximately 50–75% of Quintero stage I TTTS cases may improve with expectant management or amnioreduction. However, stage I cases with severe maternal abdominal distension, progressive polyhydramnios in the recipient twin, or cardiac dysfunction in the recipient twin may require immediate fetoscopic surgery.
Contraindications
These include:
- Severe structural abnormalities in one fetus.
- Threatened miscarriage.
- Maternal infections, especially suspected intrauterine infections.
- Total anterior placentation with no available puncture pathway.
- Severe maternal medical or obstetric complications that preclude surgical intervention.
Timing of Surgery
The optimal timing for surgery is between 16 and 26 weeks of gestation. Beyond 26 weeks, the increased size of the fetus and decreased amniotic clarity elevate the difficulty of the procedure.
Preoperative Preparation
Patients and their families are provided with an explanation of the procedure, its necessity, associated risks, and potential maternal-fetal or neonatal complications, along with alternative options. Informed consent is obtained. Routine preoperative tests include blood and urine analyses, biochemical testing, coagulation profiles, electrocardiograms, and cervical length measurement.
The surgical equipment, including an imaging system, light source, trochar, fetoscope (sheath), laser fiber, laser generator, and color Doppler ultrasound machine, is prepared.
Prophylactic antibiotics, and if necessary, uterine contraction inhibitors, are administered preoperatively.
Surgical Procedure
Local anesthesia is commonly used; however, spinal anesthesia or sedation may be required for prolonged procedures.
Access to the recipient twin's amniotic sac is established via a 2 mm or 3 mm fetoscope inserted through the maternal abdominal wall and circumventing the placenta. For anterior placentation, a 30° angled fetoscope or curved fetoscope may be employed.
The placental vessels and anastomoses are identified under direct fetoscopic visualization, based on vessel color and their trajectory from the umbilical cord root. A vascular equator is established as a guide.
Selective laser coagulation of anastomotic vessels or the Solomon technique is performed. The former targets specific A-V, V-A, A-A, and V-V anastomotic vessels sequentially. The latter connects coagulation points on the placental surface with a laser, minimizing residual small anastomoses to reduce the risks of post-surgical twin anemia-polycythemia sequence (TAPS) or reverse TTTS.
Amnioreduction is conducted postoperatively to restore amniotic fluid depth to normal levels.
Common Postoperative Complications
Maternal Complications
The overall incidence of maternal complications is 5.9%, with severe complications (e.g., placental abruption, severe infections, pulmonary edema) occurring in 1.5%. Mild complications include hemorrhage, chorioamnionitis, and amniotic fluid leakage. Postoperative management requires monitoring for maternal blood dilution and fluid intake. Risks of preterm labor, premature rupture of membranes, and miscarriage are elevated. Delivery typically occurs between 31 and 33 weeks of pregnancy. The occurrence of iatrogenic monochorionic monoamniotic twins due to amniotic membrane perforation is 20%.
Fetal Complications
Near-term complications include intrauterine death of one or both fetuses, pseudomembranous band syndrome (2.2%), fetal body or limb burns, iatrogenic twin anemia-polycythemia sequence (3–13%), and recurrent TTTS (5–10%). Long-term complications include neurological impairment in infants, partly attributable to prematurity and the pathophysiological mechanisms of TTTS itself.
In-Utero Treatment of Fetal Posterior Urethral Valves (PUVs)
Posterior urethral valves can lead to progressive oligohydramnios, pulmonary hypoplasia, and cystic renal dysplasia. Fetoscopic laser ablation of the posterior urethral valves, along with the placement of a urinary drainage stent, is a potential treatment. However, the indications for surgery and its efficacy remain to be thoroughly evaluated.
In-Utero Treatment for Severe Congenital Diaphragmatic Hernia (CDH)
Severe diaphragmatic hernia may result in significant pulmonary hypoplasia, rendering the affected neonate unlikely to survive after birth. Fetoscopic endoluminal tracheal occlusion (FETO) has improved postnatal six-month survival rates for cases with severe diaphragmatic hernia from 15% to 40%. However, whether in-utero treatment significantly reduces the incidence of neonatal pulmonary hypoplasia and improves long-term outcomes requires further investigation.
Management of Amniotic Band Syndrome (ABS)
Amniotic band syndrome refers to a spectrum of sporadic congenital structural abnormalities (involving limbs, face, and trunk) that can present as constriction bands, syndactyly, intrauterine amputations, or more complex defects involving facial structures, internal organs, and the body wall. In some cases, constriction bands may entangle the umbilical cord, resulting in fetal demise. Fetoscopic amniotic band release may prevent limb loss before irreversible fetal damage occurs; however, the indications for surgery and its effectiveness require further assessment.
In-Utero Treatment of Fetal Open Spina Bifida (Meningomyelocele, MMC)
Open MMC, characterized by spinal cord and nerve exposure to amniotic fluid, can cause a "second-hit" phenomenon during fetal development. Neurotoxic substances in the amniotic fluid impair the development of the nervous system, leading to severe, irreversible outcomes such as intellectual disability, motor dysfunction, anal sphincter incompetence, sexual dysfunction, and Chiari II malformations. Compared to open fetal surgery, fetoscopic repair of MMC is associated with fewer maternal complications, no risk of uterine scar rupture during delivery, and the option of vaginal trial of labor. However, long-term efficacy still needs confirmation through randomized controlled trials.