Gynecological imaging examinations include ultrasound (US), X-ray imaging, computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET), all of which are widely used in the field of gynecology due to their minimal invasiveness and diagnostic accuracy.
Ultrasound Examination
Ultrasound as a Common Imaging Modality in Gynecology
Ultrasound imaging techniques used in gynecology include two-dimensional imaging, three-dimensional imaging, color Doppler imaging, and contrast-enhanced ultrasound. Frequencies used for gynecological ultrasound range from 1–9 MHz, with abdominal ultrasound typically utilizing frequencies of 3–3.5 MHz, and transvaginal ultrasound employing frequencies of 5–7.5 MHz. The examination routes include transabdominal, transvaginal (or transrectal), and transperineal approaches.
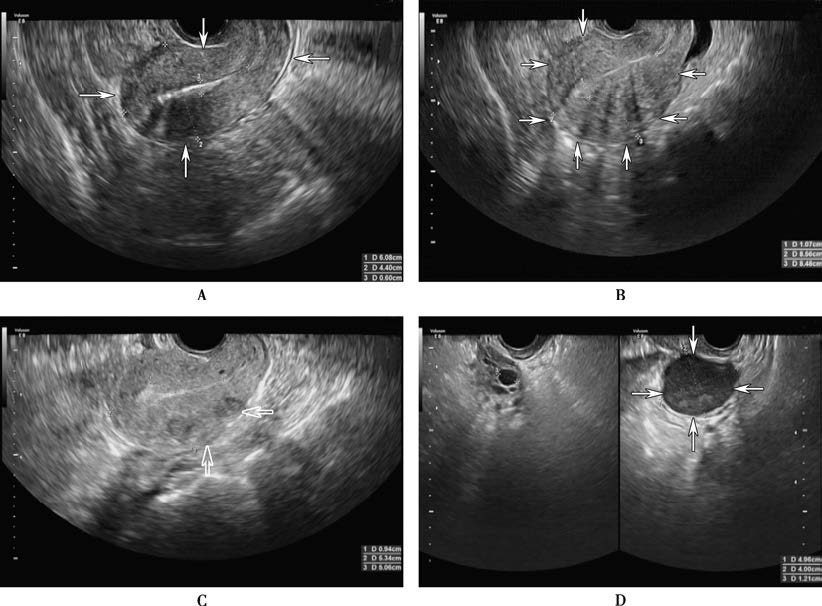
Figure 1 Gray-scale ultrasound images
A. The arrow indicates the normal uterus.
B. The arrow indicates adenomyosis lesions in the uterus.
C. The arrow indicates uterine fibroid lesions.
D. The arrow indicates a cyst in the left ovary.
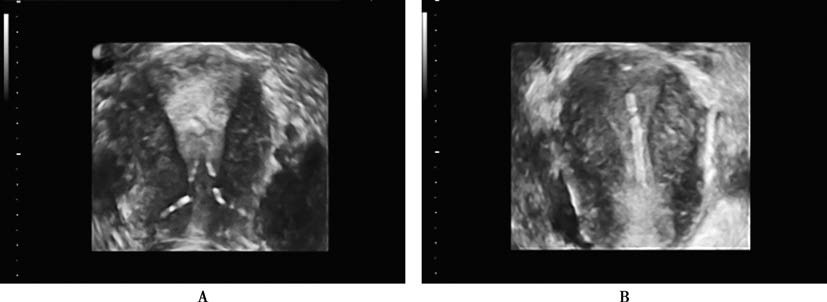
Figure 2 Three-dimensional ultrasound showing an endometrial polyp and intrauterine device
A. An inverted endometrial polyp embedded with an intrauterine device (IUD).
B. A downward displacement of the intrauterine device.
Transabdominal Ultrasound Examination
This provides a broader field of view, particularly for large masses. Pre-examination bladder filling serves as an acoustic window, ideally with the bladder level slightly higher than the uterine fundus. The patient lies in a supine position, exposing the lower abdomen, and coupling gel is applied to the skin in the examination area. The examiner scans longitudinally, transversely, and at various angles using the transducer.
Transvaginal (or Transrectal) Ultrasound Examination
This involves disinfecting the transducer, applying coupling gel, and covering the transducer with a disposable rubber sheath. Patients empty their bladder before the examination and assume the lithotomy position. The transducer is gently inserted into the vagina (or rectum), and its angle is adjusted to obtain satisfactory images. Transvaginal (or transrectal) ultrasound offers high resolution and clear images, making it particularly suitable for examining deeper pelvic organs or for patients with obesity. However, it cannot fully image masses extending beyond the pelvis. For individuals without a history of sexual activity, transrectal ultrasound is preferred.
Transperineal Ultrasound Examination
This allows scanning of the perineal area to evaluate diseases of the external genitalia, distal vagina, or other conditions affecting the pelvic floor.
Applications of Ultrasound in Gynecological Disease Diagnosis
Uterine Fibroids
Ultrasound images show an enlarged uterus, with non-degenerate fibroids presenting as round or oval hypoechoic or isoechoic areas of varying sizes and clear borders. Degenerate fibroids exhibit uneven internal echoes, which may include hypoechoic, hyperechoic, or isoechoic regions. Blood vessels in fibroids appear in a star-shaped pattern, while peri-fibroid vessels have ring-like or semi-ring distributions. Ultrasound is highly accurate in distinguishing intramural, submucosal, and subserosal fibroids. High-intensity focused ultrasound (HIFU) is used for ablative treatment of uterine fibroids.
Adenomyosis and Adenomyomas
Adenomyosis presents as diffuse uterine enlargement and heterogeneous myometrial echogenicity on ultrasound. Adenomyomas show irregularly defined hypoechoic regions within an irregularly enlarged uterus.
Pelvic Endometriosis
Ultrasound typically reveals cystic masses of varying sizes with wall thickness that may range from smooth to rough. Internal echoes appear as granular, fine signals or dense, coarse spots due to coagulated blood, and no blood flow signals are detected. Adhesion to surrounding tissues may result in unclear boundaries.
Pelvic Inflammatory Disease
Pelvic inflammatory masses adhere to surrounding tissues with poorly defined boundaries. Fluid or pus accumulation appears as anechoic or heterogeneous echo regions.
Pelvic Floor Dysfunction
Convex-array volume transducers are used to evaluate the presence of pelvic organ prolapse and other disorders.
Hydatidiform Mole
Complete hydatidiform mole is characterized by the following ultrasound features:
Uterine enlargement greater than expected for gestational age.
No fetal or associated structures within the uterine cavity.
Multiple honeycomb-like anechoic areas of varying sizes filling the uterine cavity.
Presence of single or multilocular luteinized ovarian cysts in bilateral adnexal areas.
Endometrial Cancer
Transvaginal ultrasound is preferred. Gray-scale ultrasound imaging often reveals diffuse or focal endometrial thickening and heterogeneous echogenicity. Myometrial involvement results in blurry boundaries between the endometrium and myometrium, which may show uneven hypoechoic regions. Color Doppler and spectral Doppler imaging may indicate rich or sparse blood flow patterns or normal distributions. Ultrasound is useful for assessing tumor size, location, and the extent of myometrial invasion.
Uterine Sarcoma
Ultrasound imaging shows uterine enlargement with an irregular shape, disrupted tumor echogenicity, disappearance of normal endometrial structure, and unclear boundaries with surrounding myometrium. Color Doppler imaging shows abundant, disorganized low-resistance blood flow signals within and around the tumor. Uterine sarcomas have nonspecific ultrasound features.
Cervical Cancer
Typical ultrasound features include cervical enlargement, abnormal shape, reduced echogenicity, and abundant internal blood flow. Ultrasound is helpful for assessing tumor size and the depth of stromal invasion.
Ovarian Tumors
Ultrasound images reveal information about tumor internal echogenicity, size, boundaries, and the characteristics of cyst contents. Color Doppler imaging indicates blood flow distribution within and around the tumor. These features aid in determining tumor type, anatomical location, and its relationship with surrounding tissues. Benign tumors often appear as unilocular or multilocular anechoic areas with clear boundaries and no papillary projections, while malignant tumors show irregular margins, heterogeneous internal echoes, solid components with abundant blood flow signals, and ≥4 papillary projections. Malignant tumors may also be associated with ascites or peritoneal nodules. Ultrasound is highly accurate in determining the nature of ovarian tumors.
Follicular Development Monitoring
Monitoring typically begins on the 10th day of the menstrual cycle. Normal follicles grow approximately 1.6 mm per day, reaching about 20 mm prior to ovulation.
Detection of Intrauterine Contraceptive Devices
Ultrasound accurately displays the shape and position of intrauterine contraceptive devices within the uterine cavity. It can identify device dislocation, embedment, perforation, or migration outside the uterus and assist in guided removal.
Interventional Ultrasound Applications
Transvaginal ultrasound is used for procedures such as ovum retrieval from mature follicles. Ultrasound-guided fine-needle aspiration biopsy of pelvic masses is widely applied for tissue sampling, with an overall diagnostic accuracy exceeding 90%. It may also allow medication injection for treatment. The procedure is minimally invasive with high feasibility but carries a potential risk of tumor seeding.
Contrast-Enhanced Ultrasound (CEUS)
Contrast-enhanced ultrasound (CEUS) is referred to as the "third revolution" in ultrasound technology. It is performed on the basis of conventional ultrasound by intravenously injecting an ultrasound contrast agent (microbubbles of sulfur hexafluoride). The contrast agent reaches target organs through the blood circulation, utilizing the scattering and backscattering properties of microbubbles to effectively enhance imaging of parenchymal or hollow organs and improve Doppler blood flow signals. This enables the detailed visualization of microcirculation and improves contrast resolution. CEUS serves as an important tool for the early diagnosis of gynecological tumors and for distinguishing between benign and malignant ovarian tumors, uterine fibroids, and adenomyosis.
Sonohysterography involves introducing a contrast agent (such as saline or hydrogen peroxide) into the uterine cavity to expand it and improve visualization. This method is used for evaluating endometrial lesions, submucosal fibroids, intrauterine adhesions, uterine scar diverticula following cesarean section, and congenital abnormalities of uterine development.
X-Ray Imaging
Digital Radiography (DR)
Digital radiography utilizes computer-based processing to transform analog image signals into a digital matrix through sampling and analog-to-digital conversion. It is currently the most commonly used X-ray examination in clinical practice.
Hysterosalpingography (HSG)
This imaging examination involves the introduction of iodine contrast agents into the uterus via the cervical os to evaluate the morphology of the uterine cavity and fallopian tubes. It enables the assessment of uterine position, cavity size, congenital uterine abnormalities, and tubal patency. Additionally, it may restore tubal patency by separating adhesions within the uterus or fallopian tubes, serving a therapeutic purpose in some cases.
Chest X-Ray
Chest X-ray imaging is employed for the diagnosis and monitoring of pulmonary metastases from gynecological malignancies. It is particularly useful in evaluating lung metastases of gestational trophoblastic tumors and can be used to count pulmonary metastatic lesions. However, its density resolution is relatively limited, making it less effective for detecting small pulmonary lesions. In such cases, chest X-ray imaging may be complemented with CT scanning as needed.
Colorectal Contrast Imaging
This imaging technique involves the introduction of a contrast agent into the rectum through the anus to visualize the rectal and colonic lumen. It is useful for assessing the positional relationship and degree of involvement between pelvic masses and the rectum or colon, as well as for evaluating complications such as intestinal fistulas.
Intravenous Pyelography (IVP)
Intravenous injection of a contrast agent is used to evaluate the urinary system. The contrast agent reaches the kidneys through the bloodstream and is excreted via the urinary tract, generating an image that reflects excretory function. IVP can help identify obstructions, strictures, tumors, and other abnormalities, as well as assess the positional relationships and involvement of gynecological tumors with the bladder and ureters.
Digital Subtraction Angiography (DSA)
DSA utilizes dynamic imaging under X-ray guidance. Contrast agents are introduced via catheterization into the internal iliac artery or uterine artery following percutaneous puncture of the femoral artery. This technique provides detailed visualization of vascular changes, including displacement, stenosis, dilation, deformation, twisting, erosion, neovascularization, arteriovenous fistulas, contrast agent retention, filling defects, and avascular areas. DSA contributes to the evaluation of the nature of pelvic masses and the vascular architecture within tumor lesions.
For patients with massive uterine bleeding, intra-arterial injection of embolic agents can be used to achieve hemostasis.
For chemotherapy-resistant lesions in gynecological malignancies, arterial catheterization enables the localized infusion of chemotherapeutic agents to increase local drug concentration and reduce tumor volume.
Interventional therapy using DSA is also applicable for other gynecological conditions, such as uterine fibroids and adenomyosis.
Computed Tomography (CT)
Computed tomography (CT) utilizes the varying penetration abilities of X-rays through tissues of different densities in the human body. This creates differences in the attenuation values of the received X-rays, which are processed as gray-scale images by a computer. CT provides high-resolution images, enabling the visualization of structural characteristics of tumors, their precise location, solid or cystic nature, calcifications, surrounding invasions, and distant metastases. CT is used in the diagnosis and staging of various gynecological tumors, the development of treatment plans, prognosis evaluation, assessing therapeutic efficacy, and diagnosing postoperative recurrence. However, its specificity for ovarian tumor localization and layer-specific assessment of cervical and endometrial cancer infiltration is lower compared to magnetic resonance imaging (MRI).
CT Contrast-Enhanced Scanning
Contrast-enhanced CT scanning, conducted after intravenous injection of a contrast agent, significantly improves the density contrast between pathological and normal tissues. For confirmed gynecological malignancies, enhanced CT scans of the neck, chest, abdomen, and pelvis can assess tumor location, local invasion, regional and distant metastases, as well as assist in clinical staging and treatment planning. For post-treatment patients, CT is useful for evaluating therapeutic efficacy and detecting local recurrence or metastases.
CT Angiography (CTA)
CT angiography involves intravenous injection of a contrast agent, followed by CT imaging to capture vascular structures. The technique provides three-dimensional images of arterial and venous structures in multiple planes and from various orientations. This allows for a detailed assessment of the vascular structures of organs and surrounding lesions, aiding in the evaluation of blood supply to gynecological tumors and their relationship with surrounding vasculature. Pulmonary CTA is used for diagnosing and assessing the severity of pulmonary embolism.
CT Urography (CTU)
CT urography involves intravenous injection of a contrast agent, and imaging is performed to capture the excretion process of the contrast agent through the urinary system. Post-processing reconstruction produces a three-dimensional image of the entire urinary system, assisting in the evaluation of the positional relationship and involvement of gynecological tumors with the urinary system.
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging (MRI) utilizes the resonance phenomenon of hydrogen nuclei (protons) in human tissues under a magnetic field when stimulated by radiofrequency pulses. The resulting signals are processed by a computer to reconstruct tomographic images of the body. MRI provides imaging with no radiation exposure, no osseous artifacts, and high soft-tissue resolution. It supports multi-parametric, multi-sequence, and multi-planar imaging, which allows the detailed visualization of uterine layers and ovarian structures. It is widely applied in determining the origin and extent of pelvic lesions. High-resolution imaging in both the coronal and axial planes of the uterus can reveal the signal differences between tumors and normal tissues, enabling accurate assessment of tumor size, nature, infiltration range, and metastases. As a result, MRI is broadly utilized in diagnosing gynecological diseases, evaluating therapeutic efficacy, and serving as the preferred imaging method for pre-treatment assessment, clinical staging, and post-treatment follow-up monitoring of cervical and endometrial cancers.
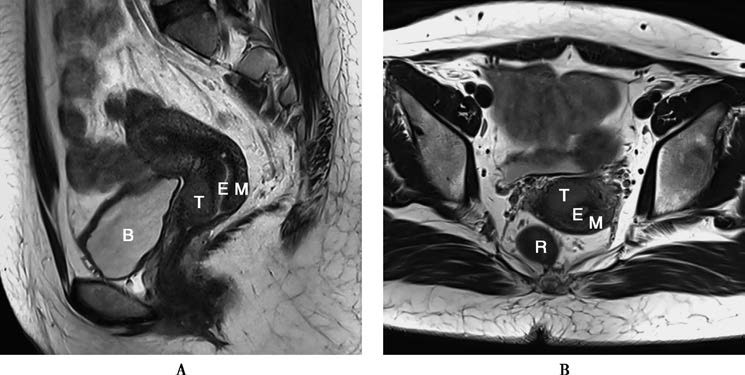
Figure 3 Magnetic resonance imaging showing cervical cancer lesions
A. Sagittal T2WI-TSE image.
B. Oblique axial T2WI-FSE image perpendicular to the uterine long axis.
M: Myometrium; E: Endometrium; T: Tumor; B: Bladder; R: Rectum.
MRI Applications in Gynecological Evaluation
MRI can clearly identify various congenital abnormalities and malformations of the female reproductive system. It provides significant advantages over CT and ultrasound in determining the origin, nature, and extent of pelvic masses. For confirmed gynecological malignancies, MRI staging accuracy surpasses that of CT and ultrasound. When metastases are suspected, abdominal MRI can accurately evaluate organ, peritoneal, lymphatic, or bone involvement, while brain MRI can assess brain metastases. Additionally, MRI is more sensitive than other modalities in evaluating the response to therapy and in differentiating post-treatment fibrosis from tumor recurrence.
Fat Suppression Techniques
Fat suppression techniques reduce the high signal intensity generated by fat components in images, which can aid in determining whether lesions contain fat components.
Magnetic Resonance Angiography (MRA)
MRA allows the detailed visualization of vasculature within and surrounding pelvic organs and lesions, and it helps in assessing vascular abnormalities such as arterial stenosis, occlusion, arteriovenous thrombosis, aneurysms, and vascular malformations. It also evaluates the blood supply to gynecological tumors and their relationships with surrounding vasculature.
Functional MRI
Functional MRI techniques enable the early diagnosis and differential diagnosis of gynecologic diseases, as well as post-treatment efficacy evaluation, by utilizing functional information before morphological changes appear in the lesion. These include diffusion-weighted imaging (DWI), perfusion-weighted imaging (PWI), and magnetic resonance spectroscopy (MRS), which have been widely applied in clinical practice.
Positron Emission Tomography (PET)
Positron emission tomography (PET) is a functional imaging technique that utilizes tracers to reveal the biochemical and metabolic processes of organs or pathological tissues. The most commonly used tracer for PET is fluorine-18-labeled deoxyglucose (18F-FDG), which accumulates in cells in proportion to their rate of glucose metabolism. Because malignant tumor cells possess significantly higher glycolytic metabolic rates compared to normal or benign cells, PET is often used for the diagnosis, differential diagnosis, evaluation of therapeutic response and prognosis, and detection of recurrence in malignant tumors.
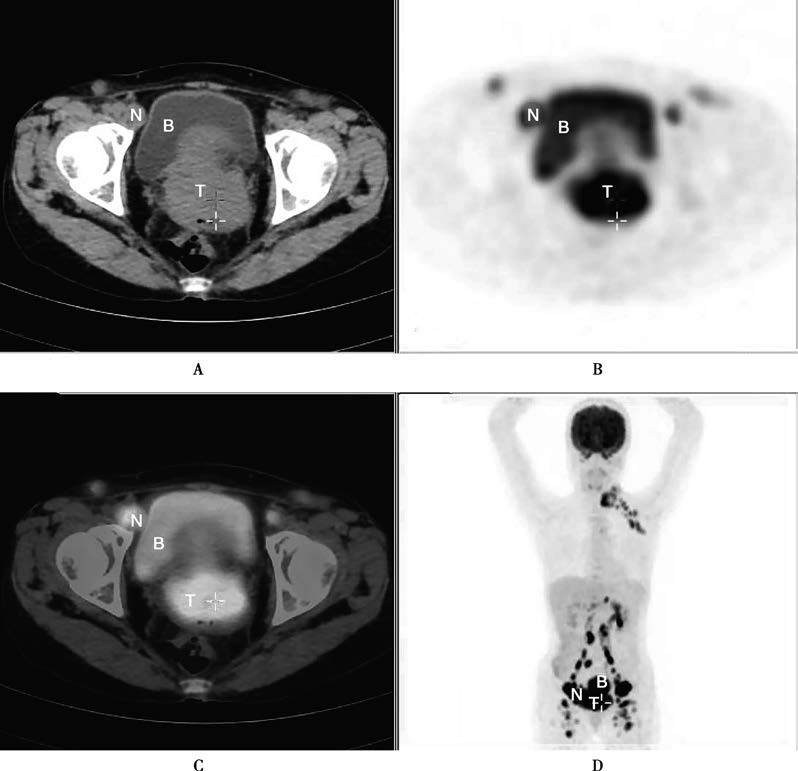
Figure 4 PET/CT showing cervical cancer with multiple lymph node metastases in the left supraclavicular region, abdominopelvic cavity, and retroperitoneum
A. Axial CT image.
B. Axial PET image.
C. Axial fusion image of PET and CT.
D. Coronal PET image.
T: Tumor; B: Bladder; N: Lymph nodes.
In the field of gynecology, PET false positives may occur in cases of endometriosis, acute pelvic inflammation, or high 18F-FDG uptake in ovarian tissues during the late menstrual phase in women of reproductive age. PET/CT combines PET and CT into a single imaging system, capturing both PET functional and CT anatomical images in one examination. The fused images simultaneously display detailed anatomical structures and functional changes within lesions, offering enhanced diagnostic accuracy. PET/CT demonstrates particular advantages over conventional imaging methods in diagnosing recurrent or metastatic lesions.