Abdominal puncture and amniocentesis are commonly employed diagnostic techniques in obstetrics and gynecology. Abdominal puncture can be performed through two approaches: transabdominal wall puncture and transvaginal posterior fornix puncture. Amniocentesis is typically conducted via a transabdominal route into the amniotic cavity.
Abdominal Puncture
Transabdominal Abdominal Puncture
Since gynecological conditions primarily involve the pelvis and lower abdomen, abdominal paracentesis is utilized to extract fluid or tissue from the pelvic-abdominal cavity to achieve diagnostic and therapeutic purposes. The color, concentration, and viscosity of the aspirated fluid are closely examined, while specimen tests—such as routine laboratory tests, cytology, bacterial culture, and drug sensitivity tests—are conducted to identify the characteristics of the fluid in the pelvic/abdominal cavity or to detect tumor cells. Additionally, under ultrasound guidance, fine-needle aspiration biopsy may be performed on pelvic or lower abdominal masses for histological evaluation.
Indications
This is indicated:
- To assist in diagnosing and determining the nature of abdominal fluid accumulation.
- To identify the nature of masses located near the abdominal wall in the pelvis and lower abdomen.
- To aspirate and drain abdominal fluid, which softens the abdominal wall for pelvic-abdominal examinations or alleviates symptoms such as abdominal distension and respiratory distress.
- To facilitate intraperitoneal chemotherapy by injecting chemotherapeutic drugs during the procedure.
- To introduce CO2 gas into the abdominal cavity for pneumoperitoneal X-ray imaging, which provides clear visualization of pelvic organs.
Contraindications
These include:
- Suspected severe adhesions or bowel obstruction in the abdominal cavity.
- Suspected giant ovarian cysts.
- Psychologically unstable or uncooperative patients.
- Pregnant patients in the second or third trimester.
- Patients with disseminated intravascular coagulation.
Procedure
For ultrasound-guided transabdominal aspiration, the procedure often begins with bladder filling to confirm the location of the mass, followed by bladder emptying before puncture. For transvaginal ultrasound-guided aspiration, the bladder is emptied prior to the procedure.
Patients lie supine when there is a significant amount of abdominal fluid or when aspirating a cyst. When fluid volume is small, a semi-recumbent or lateral-tilted position may be adopted.
The puncture site is typically located at the junction of the middle and outer one-third of the line connecting the umbilicus and the left anterior superior iliac spine. For cyst aspiration, the puncture site is selected at the most prominent cystic area.
The puncture area is routinely disinfected, and a sterile drape is applied. The clinician wears sterile gloves.
Local infiltration anesthesia is performed using 0.5% lidocaine, administered in layers from the skin to the parietal peritoneum.
A 7G puncture needle is vertically inserted into the abdominal cavity at the selected site. A loss of resistance indicates entry into the peritoneum. The needle is stabilized using sterile hemostatic forceps, and the stylet is removed. Upon observing fluid outflow, a syringe is used to aspirate sufficient fluid for examination. Cytological examination typically requires 100–200 mL of fluid, while other tests may only need 10–20 mL. For fluid drainage, the needle is connected to a catheter, with the other end leading to a collection container. The amount of fluid drained and the catheter placement duration are determined based on the patient’s clinical condition and diagnostic/therapeutic needs. If assessing for tumors in the pelvic cavity, drainage may continue until the abdominal wall softens and is suitable for examination.
Fine-needle aspiration biopsy is performed using specifically designed needles, under ultrasound guidance, to extract a small tissue sample from the lesion for histological examination.
Upon completion of the procedure, the puncture needle is withdrawn, the area is disinfected again, and a sterile dressing is applied and secured. If fluid leakage occurs from the puncture site, gentle pressure may be applied.
Characteristics of Fluid and Interpretation of Results
Blood
Fresh blood that clots quickly indicates vascular injury; adjustment in needle direction or repeat puncture may be required.
Dark red, non-coagulated blood persisting after 10 minutes suggests internal bleeding, commonly seen in ectopic pregnancy, ovarian corpus luteum rupture, or rupture of other organs such as the spleen.
Small blood clots or non-coagulated, dark red blood suggest chronic ectopic pregnancy.
Chocolate-colored, viscous fluid with unformed debris under microscopy indicates ruptured ovarian endometriotic cysts.
Pus
Yellow, yellow-green, or light chocolate-colored, either thin or thick with a foul smell, suggests purulent lesions in the pelvis or abdomen, such as abscess rupture. Cytological smears, bacterial culture, and drug sensitivity testing are necessary for further evaluation.
Inflammatory Exudate
Pink or pale yellow turbid fluid suggests pelvic or abdominal inflammation. Cytological examination, bacterial culture, and drug sensitivity testing are recommended.
Ascitic Fluid
Bloody, serous, or mucus-like fluid requires routine laboratory tests, including specific gravity, total cell count, red and white blood cell counts, protein levels, Rivalta’s test, and cytological examination. Acid-fast bacilli and Mycobacterium tuberculosis culture or animal inoculation may be conducted if necessary. Hemorrhagic ascites often suggests malignant tumors, warranting exfoliative cytology.
Precautions
Preoperative patient assessment includes monitoring vital signs, measuring abdominal circumference, and examining abdominal symptoms.
Aseptic technique is imperative to prevent abdominal cavity infection.
The depth of needle insertion is controlled to avoid damaging blood vessels or intestines.
Stabilizing the needle is critical during large-volume drainage to prevent needle displacement or intestinal injury. Fluid drainage should proceed at a controlled rate, with no more than 1,000 mL aspirated per hour and no more than 3,000 mL aspirated in total per session. Vital signs, including blood pressure, pulse, and respiration, are closely monitored, and fluid drainage is adjusted accordingly if signs of shock occur. Gradual abdominal band compression is applied during the procedure to prevent abrupt intra-abdominal pressure drops, which can lead to visceral vasodilation and shock.
Careful consideration must be given to any medication injected into the peritoneal cavity, as many drugs are contraindicated for this administration route. When performing intraperitoneal chemotherapy, potential allergic and toxic reactions should be monitored.
Patients are advised to rest in bed for 8–12 hours after the procedure, and prophylactic antibiotics may be prescribed to prevent infection, if necessary.
Transvaginal Posterior Fornix Puncture
The recto-uterine pouch represents the lowest point in the abdominal cavity, where accumulations of blood, fluid, or pus often collect. The top of the vaginal posterior fornix is closely adjacent to the recto-uterine pouch, and the technique of transvaginal posterior fornix puncture (culdocentesis) is commonly employed in obstetrics and gynecology. This procedure involves aspirating content from the posterior fornix for macroscopic observation, laboratory examination, and pathological analysis as an auxiliary diagnostic method.
Indications
These include:
- Suspected intra-abdominal bleeding, such as in cases of ectopic pregnancy or ovarian corpus luteum rupture.
- Suspected accumulation of fluid or pus in the pelvic cavity; fluid aspiration is performed to determine the nature of the accumulation, to puncture and drain pelvic abscesses, or to administer local medication.
- Cases of pelvic masses located in the recto-uterine pouch; direct aspiration through the posterior fornix may be employed for cytological and histological analysis (Fine-needle aspiration is preferred for suspected malignancies, while caution is required for cystic lesions to prevent tumor seeding).
- Ultrasound-guided drug injection for ovarian endometriotic cysts or treatment of tubal ectopic pregnancies.
- Oocyte retrieval via ultrasound-guided transvaginal posterior fornix puncture as part of assisted reproductive technologies.
Contraindications
These include:
- Severe pelvic adhesions occupying the recto-uterine pouch with tissue masses extending toward the rectum.
- Suspected adhesion of the intestine to the posterior uterine wall, where puncture may risk intestinal or uterine injury.
- Planned non-surgical treatment of ectopic pregnancy due to the risk of infection.
Procedure
After bladder emptying, the patient is placed in the bladder lithotomy position. Routine disinfection of the external genitalia and vagina is performed, followed by draping. A bimanual examination is used to assess the uterus, adnexa, and the presence of bulging at the vaginal posterior fornix.
The cervix and posterior vaginal fornix are exposed using a vaginal speculum and disinfected. The posterior lip of the cervix is held with a tenaculum and pulled forward to fully expose the posterior fornix. Disinfection is repeated.
Using a lumbar puncture needle or a long 22-gauge needle attached to a 5–10 mL syringe, the central posterior fornix or the most prominent side (adjacent to the affected area, if relevant) is punctured. This point is slightly below the junction of the posterior vaginal wall and posterior lip of the cervix, with the needle aligned parallel to the uterine canal. The needle is quickly advanced 2–3 cm. A sensation of tissue yielding indicates entry into the cavity, at which point aspiration is initiated. If no fluid is aspirated, the syringe is continually withdrawn while aspirating; redirection may be required if necessary. If fluid appears in the syringe, retraction is stopped, and the appropriate amount of fluid is aspirated for laboratory analysis. For fine-needle aspiration biopsy, a specialized puncture needle is used, following the same technique.
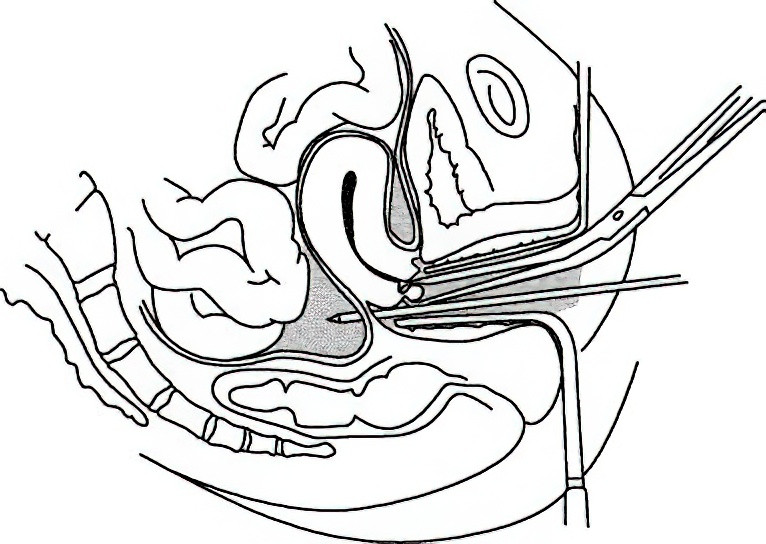
Figure 1 Transvaginal posterior fornix puncture
After completing the aspiration, the needle is withdrawn. If active bleeding is observed at the puncture site, gentle pressure using a cotton ball is applied until bleeding ceases. The vaginal speculum is subsequently removed.
Characteristics of the Fluid and Interpretation of Results
The characteristics of the aspirated fluid and the methods of result interpretation are essentially the same as for transabdominal abdominal puncture.
Precautions
The puncture site is located at the central posterior fornix or slightly off the affected side at the most prominent point. Needle direction aligns parallel to the uterine canal and extends into the recto-uterine pouch without excessive forward or backward deviation to avoid piercing the uterine body or rectum.
Needle depth must be appropriate, generally 2–3 cm. Excessive depth risks penetrating pelvic organs or blood vessels. When fluid volume is low, an overly deep needle may exceed the fluid level, leading to failed aspiration and delayed diagnosis.
If the aspirated material is blood, it should be left to sit for five minutes; coagulation suggests intravascular blood. Alternatively, the appearance of a reddish halo on gauze indicates intravascular blood. Non-coagulated blood after six minutes is indicative of intra-abdominal bleeding.
When feasible and clinically permissible, ultrasound examination prior to the procedure aids in diagnosing the presence and volume of fluid in the recto-uterine pouch.
Failure to aspirate blood during a posterior fornix puncture does not completely rule out ectopic pregnancy or intra-abdominal bleeding. Small internal bleeds, high-positioned hematomas, or adhesions to surrounding tissues may lead to false negatives.
Depending on preliminary diagnosis, aspirated fluid should undergo smearing, routine tests, sensitivity testing, cytological examination, and other relevant analyses. Aspirated tissue should be submitted for histological examination.
Transabdominal Amniocentesis
Transabdominal amniocentesis is a technique performed in the mid-to-late stages of pregnancy. This involves using a puncture needle to access the amniotic cavity through the abdominal and uterine walls. The procedure allows for the aspiration of amniotic fluid for clinical analysis and diagnosis, or for the injection of medication or saline solutions for therapeutic purposes.
Indications
Indications for therapeutic use include:
- Administration of intra-amniotic medications (e.g., ethacridine) for termination of pregnancy due to fetal abnormalities or fetal demise.
- Induction of fetal lung maturity in cases where the pregnancy must be terminated urgently, involving intra-amniotic injection of 10 mg dexamethasone.
- Symptomatic improvement and pregnancy extension in non-anomalous fetuses with polyhydramnios by releasing an appropriate amount of amniotic fluid, thereby improving fetal survival rates.
- Management of oligohydramnios in non-anomalous fetuses by intermittent intra-amniotic injection of 0.9% sodium chloride solution to prevent placental and umbilical cord compression, reduce risks of fetal lung hypoplasia, or fetal distress.
- Treatment of complications such as maternal-fetal blood group incompatibility or twin-to-twin transfusion syndrome.
- Selective fetal reduction in cases of multifetal pregnancies.
Indications for prenatal diagnosis include:
- Chromosomal karyotyping, gene detection, and gene product analysis of amniotic fluid cells. High-risk pregnancies with suspected fetal abnormalities, based on prenatal screening, can undergo amniotic fluid sampling to determine the fetal sex and confirm the presence of chromosomal disorders or genetic diseases.
Contraindications
For intra-amniotic medication for termination of pregnancy:
- Active or severely impaired function of the heart, liver, lungs, or kidneys.
- Acute stages of various diseases.
- Presence of acute genital tract infections.
- Body temperature exceeding 37.5°C twice within 24 hours prior to the procedure.
For prenatal diagnosis:
- History of threatened miscarriage.
- Body temperature exceeding 37.5°C twice within 24 hours prior to the procedure.
Preoperative Preparation
Gestational Age
For induction of labor due to fetal abnormality, the optimal timing is 16–26 weeks of gestation.
For prenatal diagnosis, the optimal timing is 16–22 weeks of gestation. During this period, the uterine contour is well-defined, there is a relatively larger volume of amniotic fluid, sampling is easier, fetal injury is less likely, and high viability of amniotic fluid cells increases success rates for cell culture.
Puncture Site Localization
Manual Localization
An assistant stabilizes the uterus, and the puncture point is selected at a region with a prominent cystic sensation, located 2–3 transverse fingers below the uterine fundus, at the midline or either side.
Ultrasound Localization
Prior to the procedure, the placenta and an amniotic fluid pocket are identified and marked for reference. Puncture is performed in a region with ample amniotic fluid, avoiding the placenta. Direct ultrasound guidance may be used during the procedure.
Pre-Labor Induction Preparation in Mid-Pregnancy
Blood pressure, pulse, and temperature are assessed, along with general and gynecological examinations to check for pelvic tumors, uterine anomalies, or cervical development issues.
Laboratory tests include blood routine, urine routine, coagulation function, platelet count, and liver function assessments.
Perineal hair is removed as part of the procedure preparation.
Procedure
The patient urinates before being positioned supine. The puncture site is marked, and the abdominal skin is disinfected following standard protocols, with a sterile drape applied to the area. Local infiltration anesthesia with 0.5% lidocaine is administered at the puncture site. Using a 22- or 20-gauge lumbar puncture needle, vertical insertion through the abdominal wall is performed. Loss of resistance upon initial advancement indicates entry into the abdominal cavity. Further advancement results in a second resistance indicating entry into the uterine wall, followed by a second loss of resistance signifying entry into the amniotic cavity. Withdrawal of the stylet confirms successful puncture with the appearance of amniotic fluid. The required volume of amniotic fluid is aspirated or medication is directly administered. The stylet is reinserted into the needle before its removal. A sterile dry gauze is applied to the puncture site with manual pressure for 5 minutes, followed by adhesive tape fixation.
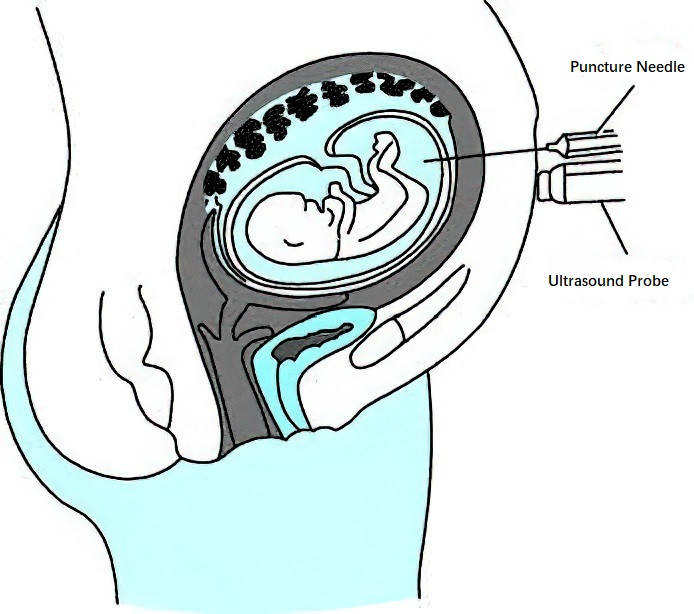
Figure 2 Transabdominal amniocentesis
Precautions
Strict adherence to aseptic techniques to prevent infection is essential.
A fine needle is preferred. Excessive needle depth or force should be avoided, and efforts should aim for success on the first attempt, with a maximum of three attempts permitted.
The location of the placenta should be determined before puncture to avoid injuring it. Amniotic fluid embolism may occur if the needle pierces the placenta, allowing amniotic fluid to enter maternal circulation through the puncture site. Before and after puncturing or withdrawing the needle, maternal symptoms such as respiratory distress and cyanosis should be closely monitored for signs of amniotic embolism.
Needle blockages caused by particulate matter in the amniotic fluid may prevent aspiration. Adjusting the puncture angle or depth usually addresses this issue. Use of a needle with a stylet minimizes such occurrences.
Aspiration of blood may indicate bleeding from the abdominal wall, uterine wall, placenta, or fetal vessels. The needle should be immediately withdrawn, and the puncture site should be compressed and bandaged. Re-puncture may be attempted after one week if there are no significant fetal heart abnormalities.
Medical staff should carefully observe potential complications post-procedure to ensure patient safety.