Female sexual dysfunction (FSD) refers to difficulties occurring in one or more phases of the female sexual response cycle or pain associated with sexual activity, which hinder the physiological sexual responses and sexual pleasure necessary for satisfactory intercourse. This condition often leads to distress or interpersonal difficulties. Due to the lack of standardized diagnostic criteria and objective evaluation metrics compared to men, reported prevalence rates of FSD vary widely. The overall prevalence of FSD is approximately 40%, with rates exceeding 50% among perimenopausal and postmenopausal women. However, only about 10% of affected women experience significant psychological distress.
Classification and Clinical Features
The classification of FSD is generally based on the phases of the sexual response cycle. Several international classification systems exist, including the World Health Organization's International Classification of Diseases-11 (ICD-11), the Diagnostic and Statistical Manual of Mental Disorders (DSM) published by the American Psychiatric Association, and the Consensus-based Classification of Female Sexual Dysfunction (CCFSD). Variations in classification standards have implications for the reported prevalence of FSD, the grouping of affected populations, and the evaluation of treatment outcomes.
The 2019 guidelines from the American College of Obstetricians and Gynecologists (ACOG) adopted the DSM-5 criteria, outlining four types of FSD. The guidelines also include two additional categories: "other specified sexual dysfunction" and "unspecified sexual dysfunction."
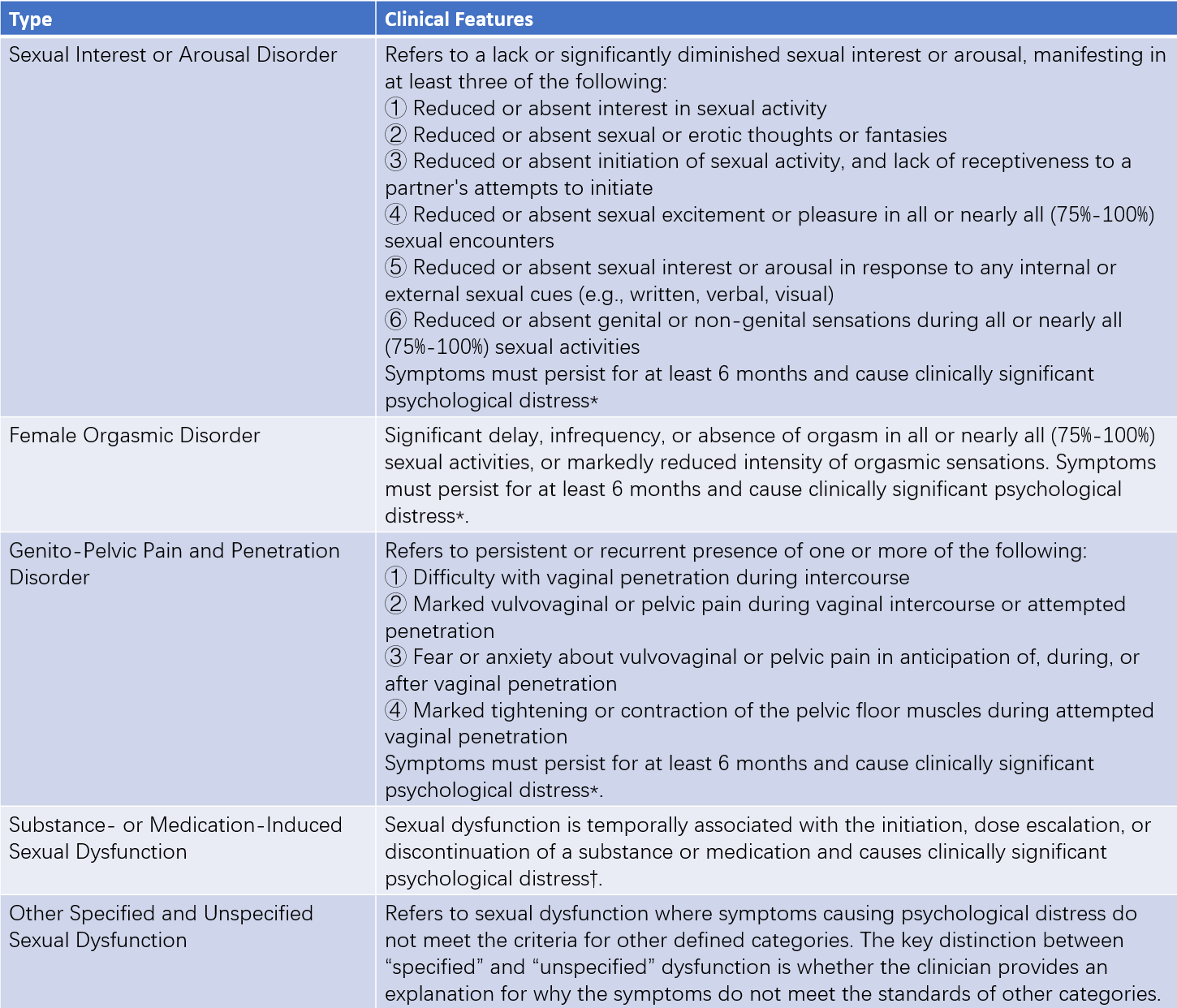
Table 1 Classification and clinical features of female sexual dysfunction
Note:
*The symptoms mentioned above cannot be explained by non-sexual mental disorders, relationship discord (e.g., issues like partner violence), or other significant stressors. They also cannot be attributed to the effects of substances, medications, or other medical conditions.
†This dysfunction cannot be better explained by another distinct sexual dysfunction. Evidence indicating non-substance- or medication-induced sexual dysfunction includes an independent history of sexual dysfunction, symptoms predating substance or medication use, or symptoms persisting for a minimum of 1 month following acute withdrawal or severe intoxication.
Contributing Factors
FSD is associated with a wide range of social, psychological, endocrine, anatomical, physiological, biochemical, and environmental factors, with psychosocial influences playing a particularly significant role.
Psychosocial Factors
Emotional factors such as shyness, depression, anxiety, fear, tension, resentment, and grief are all capable of suppressing female sexual desire and arousal. The social or personal contexts contributing to these psychological responses may include religious or traditionally conservative cultural norms, past traumatic or distressing sexual experiences, marital discord, excessive stress, concerns about pregnancy, or fears of sexually transmitted diseases.
Age and Menopause
Aging, particularly after menopause, can lead to atrophic changes in the reproductive tract, reduced pelvic blood flow, decreased pelvic floor muscle tone, and vaginal dryness, all of which can affect the sexual response. However, some epidemiological studies indicate that menopause does not significantly influence sexual activity or satisfaction, with differences potentially attributable to factors such as ethnicity and cultural background of the study population.
General or Local Health Issues
Poor overall or localized health is a common contributor to sexual dysfunction. Sexual and reproductive functions, being higher-order human needs, are often suppressed when optimal health is compromised.
Surgical Factors
Bilateral oophorectomy (removal of both ovaries) is one of the most common surgical causes of FSD. Radical vulvectomy can significantly impact sexual function by directly disrupting the anatomy of the external genitalia. Uterine and vaginal surgeries can also affect sexual function due to changes in vaginal anatomy, pelvic blood flow, or nerve damage in the pelvic region. Furthermore, mastectomy can affect sexual function due to alterations in erogenous zones, changes in body image, or psychological factors.
Radiotherapy Factors
Radiotherapy for tumors may lead to damage to ovarian function, vaginal adhesions, or changes in vaginal elasticity, all of which can impact sexual function.
Pregnancy and Postpartum Factors
During pregnancy, concerns about the fetus and changes in body image may decrease sexual function. In the postpartum period, factors such as perineal pain, reduced vaginal secretions, and incomplete recovery of the reproductive organs can lead to diminished sexual desire and arousal in women.
Medication Factors
Drugs that alter mental state, neural transmission, reproductive system blood flow, vascular function, or sex hormone levels (including alcohol) may impact female sexual function. The prevalence of medication-induced FSD is approximately 20%.
Lack of Sexual Knowledge and Skills
Insufficient understanding of female sexual response characteristics, inadequate sexual stimulation or communication skills, as well as selecting unsuitable times or locations for intimacy, may contribute to FSD.
Diagnosis
Although various objective or quantitative physical methods are available to measure female sexual response, the diagnosis of female sexual dysfunction (FSD) is currently based mainly on medical history, sexual function assessments, and physical examinations. Gynecological examinations are essential to exclude organic lesions of the reproductive tract. There are no minimum threshold criteria for frequency or severity, and the patient's cultural, religious, and social context should be considered. Attention must also be paid to whether the symptoms have caused psychological distress to the individual or negatively affected interpersonal relationships with sexual partners.
Medical History Collection
Medical history is primarily gathered through self-assessment questionnaires. These include information about the patient's age, educational background, occupation, religious beliefs, gender identity, sexual orientation, previous sexual experiences, menstrual and reproductive history, history of psychological and systemic illnesses, surgical history, history of chemotherapy or radiotherapy, history of trauma, history of medication use, and possible substance abuse. The comfort and privacy of the environment should be ensured during history collection.
Sexual Function Assessment
The use of localized and culturally adapted questionnaires is particularly important. The most commonly used international tool is the Female Sexual Function Index (FSFI), which evaluates female sexual function through 19 questions across six domains: sexual desire, sexual arousal, vaginal lubrication, orgasm, sexual satisfaction, and sexual pain. Lower scores indicate more severe sexual dysfunction. The FSFI has been demonstrated to have good reliability and validity, with high sensitivity and specificity, and is widely used in both epidemiological surveys and clinical diagnoses of sexual dysfunction. For sexually active women with pelvic floor dysfunction disorders, specific questionnaires such as the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ) or its short form (PISQ-12) are recommended.
Evaluation of Emotional and Related Issues
Emotional aspects, such as satisfaction with a marriage or relationship, emotional connection with the sexual partner, self-confidence in one's body during sexual activities, and the ability to communicate sexual needs with the partner, are evaluated.
Psychological Assessment
Psychological assessments focus on the evaluation of various psychosocial conditions related to sexual function.
Gynecological and General Physical Examination
Gynecological examinations are necessary to assess the development of reproductive organs and rule out any organic abnormalities. The examination should also consider structural and functional changes in the pelvic floor tissues. Additionally, the cardiovascular, respiratory, musculoskeletal, neurological, gastrointestinal, and urinary systems should be assessed as part of the general physical examination.
Laboratory Examinations
Current methods for assessing female sexual response include genital blood flow measurement, vaginal volume, pressure, and compliance testing, assessment of vaginal lubrication, pelvic floor muscle tension analysis, and brain functional magnetic resonance imaging (fMRI). While these methods allow for objective and even quantitative evaluations, there is often a mismatch between subjective sexual arousal and objective physiological responses in women. Female sexual satisfaction relies significantly more on subjective experiences, which reduces the necessity of laboratory testing in the initial evaluation of FSD. Laboratory tests are generally reserved for cases where an undiagnosed medical condition is suspected, or when abnormalities are identified in specialized examinations, as the clinical significance of many physical measurements remains limited.
Tests of sex hormone levels, evaluations for systemic conditions such as hypertension and diabetes, and neurological assessments are useful for identifying underlying organic conditions.
Treatment
The treatment of female sexual dysfunction (FSD) must take into full account the complexity of the female sexual response and its subjective nature, rather than relying solely on objective physiological indicators.
Psychotherapy
A comprehensive understanding of the patient's condition and the specific type of sexual dysfunction is essential for developing an effective treatment plan. The patient's type and extent of sexual psychological issues are analyzed, along with individual personality traits, cultural background, and religious beliefs. Personalized therapeutic approaches are then formulated. Including the sexual partner in psychotherapy is encouraged.
General Therapy
General approaches involve providing fundamental knowledge and practical skills related to sexuality. Reading professional books on sexual education is recommended to address and correct misunderstandings about sexuality caused by social misconceptions. Communication between partners during sexual activities is emphasized, with suggestions to explore changes in sexual positions, timing, and location. Techniques like sexual fantasy, background music, videos, or the use of lubricants may also be introduced to enhance the experience.
Behavioral Therapy
Based on classical conditioning and sociological theories, behavioral therapy targets the correction of maladaptive behaviors. Common methods include:
Sensate Focus Training
This involves focusing on subjective sensual experiences and is conducted in three stages. During the first stage, the focus is on guiding the woman to concentrate on sensations arising from her partner's physical touch, excluding the genitals and breasts. The second stage involves genital stimulation but avoids intercourse. The third stage, also known as the non-demand intercourse stage, involves transitioning to sexual intercourse on the basis of a positive response to genital stimulation. The emphasis is placed on non-demanding sexual experiences (without aiming for orgasm) and on tuning the focus toward pleasurable sensations.
Self-Stimulation Training
Patients are guided to achieve orgasm through masturbation or with the aid of vibrators. Experiencing successful orgasms helps enhance sexual desire and build self-confidence. After the patient succeeds in self-stimulation, the sexual partner can be involved to share in the experience of orgasms.
Pelvic Floor Muscle Exercises
Patients practice alternating contraction and relaxation of pelvic floor muscles to improve muscle tone and increase vaginal sensitivity during sexual activity.
Desensitization Therapy
Also called vaginal dilation therapy, this approach addresses issues with penetration. A series of vaginal dilators of increasing sizes, or the patient’s or partner's fingers, are used to gradually expand the vaginal opening.
Pharmacological Therapy
Medications may be considered when general treatments are ineffective or behavioral therapy is deemed unsuitable.
Peripheral-Acting Medications
These drugs work by relaxing vascular smooth muscles and improving blood flow, which enhances genital engorgement and vaginal lubrication. Examples include phosphodiesterase type-5 inhibitors, prostaglandin E1 agonists, and L-arginine. However, these medications are less effective in women than in men.
Central-Acting Medications
Since female sexual experiences often rely more heavily on subjective arousal, medications targeting the central nervous system may be more appropriate for women than men. Examples include melanocortin receptor agonists and dopamine receptor agonists.
Sex Hormones
Androgen therapy, whether for pre- or post-menopausal women, can significantly improve sexual desire and satisfaction. However, long-term use carries potential side effects, such as masculinization and cardiovascular risks. Estrogens and estrogen receptor modulators can help alleviate vaginal dryness. Hormones can be administered systemically or locally, depending on the medical requirements.
Antidepressants
Medications that enhance dopamine activity or suppress serotonin and prolactin can increase sexual desire. Examples include bupropion, trazodone, and fluoxetine.
Treatment of Underlying Conditions
Many cases of FSD are caused by underlying organic conditions. Proper treatment of these primary diseases can help resolve sexual dysfunction.