Primary vaginal carcinoma (PVC) is rare and accounts for only 1–2% of malignant tumors of the female genital tract and approximately 10% of malignant vaginal tumors. Primary vaginal carcinoma refers to cancer strictly confined to the vagina, with no clinical or histological evidence of cervical or vulvar cancer, and no history of cervical or vulvar cancer within the past five years.
Associated Factors
The exact cause of the disease remains unclear. Most cases of vaginal cancer are associated with persistent infection by high-risk HPV types, primarily HPV-16 and -18. Other associated factors include repeated trauma to the vaginal wall, the use of immunosuppressants, smoking, a history of cervical radiotherapy, and chronic irritation from abnormal vaginal discharge. Approximately 40% of patients with primary vaginal carcinoma have a history of total hysterectomy, with 20–30% of these cases due to hysterectomy performed for cervical precancerous lesions.
Pathology
Ninety percent of primary malignant vaginal tumors are squamous cell carcinomas, most of which are related to HPV. Vaginal adenocarcinoma accounts for around 8–10% of cases and is mostly unrelated to HPV. Rare pathological types include vaginal melanoma, lymphoma, and sarcoma.
Routes of Metastasis
The primary metastasis routes of vaginal cancer are local direct invasion and lymphatic spread, with hematogenous spread being less common.
Direct Invasion
Most vaginal tumors are located in the upper one-third of the posterior wall of the vagina. Tumors can invade surrounding pelvic soft tissue, including the paravaginal tissue, parametrium, urethra, bladder, and rectum.
Lymphatic Spread
The lymphatic drainage of the vagina is complex. Lymphatic drainage from the upper vagina reaches pelvic lymph nodes, including obturator, internal iliac, and external iliac lymph nodes, with rare metastasis to para-aortic nodes. The lower vagina drains into the inguinal lymph nodes, while middle-third lesions may drain to both pelvic and inguinal lymph nodes.
Hematogenous Spread
Advanced cases may metastasize via the bloodstream to the lungs, liver, bones, and other distant organs.
Clinical Presentation
Early symptoms of vaginal cancer may include increased vaginal discharge, irregular bleeding, or contact bleeding. Gynecological examination may reveal no visible tumor in the vagina, but white plaques or polyp-like lesions may be seen. Vaginal wall lesions may appear as nodular, cauliflower-shaped, ulcerative, or superficially eroded, with no tumorous changes in the cervix. Late-stage symptoms often resemble cervical cancer, with involvement of adjacent tissues and organs, leading to symptoms such as lower abdominal pain, lumbosacral pain, dysuria, hematuria, rectal fullness, difficulty in defecation, and pain during defecation. Inguinal, supraclavicular lymph node involvement, and distant organ metastases may also occur. Tumors infiltrating deeper layers of the vaginal wall may penetrate the posterior urethral wall or the anterior rectal wall, resulting in urinary or fecal leakage. Physical examination may reveal enlarged superficial lymph nodes, pelvic tenderness, or signs of bone metastasis. Gynecological examination may find the vagina completely occupied by the tumor, tumor infiltration into paravaginal tissues forming a frozen pelvis, or fistulas in the anterior or posterior vaginal wall.
Diagnosis
Preliminary diagnosis is made based on clinical presentation and ancillary tests, while confirmation requires histopathological examination. Diagnosis includes pathological confirmation and clinical staging. Primary malignancy of the vagina can only be diagnosed after excluding metastatic vaginal tumors originating from other sites.
Differential Diagnosis
Differential diagnoses include vaginal epithelial atrophy, vaginal condyloma acuminata, vaginal tuberculosis ulcers, and vaginal endometriosis.
Staging
Staging of primary vaginal carcinoma follows the FIGO 2009 clinical staging system. A comparison of the FIGO and AJCC-TNM 2017 staging systems is shown in Table 1.
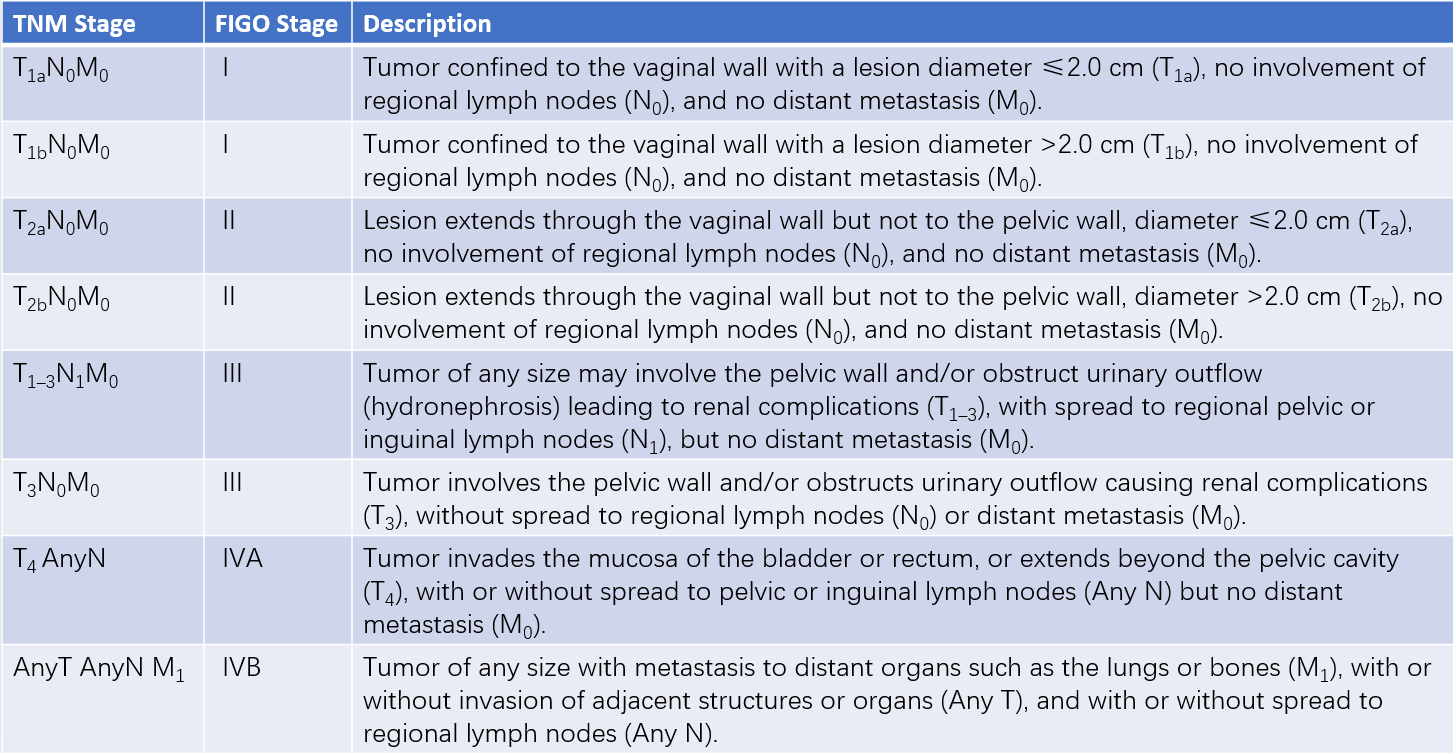
Table 1 Vaginal cancer staging
Treatment
There is currently no standardized treatment protocol for malignant vaginal tumors. Clinical management depends on factors such as pathological type, tumor size, anatomical location of the lesion, stage of the disease, and patient age. Treatment options include surgery, radiation therapy, medical therapy, or a combination of these approaches. Due to the tumor's location in the vagina, both surgical and radiotherapeutic interventions may affect fertility and sexual function.
Surgical Treatment
The role of surgery in the treatment of primary vaginal carcinoma is limited due to the proximity of lesions to the urethra, bladder, and rectum. Surgery as the initial treatment is mainly suitable for early-stage tumors confined to small lesions in the vaginal wall (less than 2 cm in size). Additional surgical indications include ovarian transposition before radiotherapy, laparoscopic removal of enlarged lymph nodes for staging purposes, or palliative procedures such as urinary diversion or colostomy for late-stage (Stage IV) or recurrent cases aimed at improving quality of life before radiotherapy.
Radiation Therapy
Radiation therapy is critical for the majority of patients, especially those with advanced-stage disease. A combination of external beam radiation therapy (EBRT) and intracavitary brachytherapy is commonly applied. CT and/or MRI-guided conformal brachytherapy can enhance the radiation dose to residual tumor tissue while minimizing exposure to and protecting surrounding healthy organs. Intensity-modulated radiation therapy (IMRT) allows for higher radiation doses to the lesion with lower doses to adjacent organs, reducing complications. Based on cervical cancer treatment protocols, concurrent chemoradiotherapy is also used for vaginal carcinoma.
Other Treatments
Chemotherapy alone shows limited efficacy and is primarily used in combination with radiation therapy or as part of a multimodal treatment approach. Chemotherapy regimens are similar to those used for vulvar carcinoma. Targeted therapy and immunotherapy can be considered based on experience derived from cervical cancer treatment strategies.
Prognosis
The main factor affecting the prognosis of vaginal cancer is disease stage. Early-stage (Stages I or II) vaginal squamous cell carcinoma is associated with a relatively favorable outcome. Poor prognostic factors include larger tumor size (greater than 4 cm), lesions extending beyond the upper one-third of the vagina, HPV status, and a high Ki-67 index. Other variables such as patient age, fertility preservation, and general health status can influence treatment selection and subsequently affect prognosis. The five-year survival rate for vaginal squamous cell carcinoma ranges from 35% to 78%, with Stage I at 85%, Stage II at 78%, and Stages III–IVA at 58%.
Follow-Up
It is recommended that during the first year following treatment, follow-up visits are scheduled every 1–3 months; during the second and third years, follow-up is conducted every 3–6 months; and after the third year, follow-up is conducted annually. During follow-up, vaginal cytological assessments and HPV testing should be performed, with colposcopy and imaging studies conducted as needed.